Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,533

And the Covid wave in England continues...
The Covid summer goes on.

Christina Pagel
Aug 01, 2024
40
4
Share
Current levels of Covid
Sadly, the current Covid “FLiRT” variants aren’t relaxing their grip.According to the latest UKHSA data, hospital admissions with Covid decreased very slightly in the previous week but admission levels remain high.
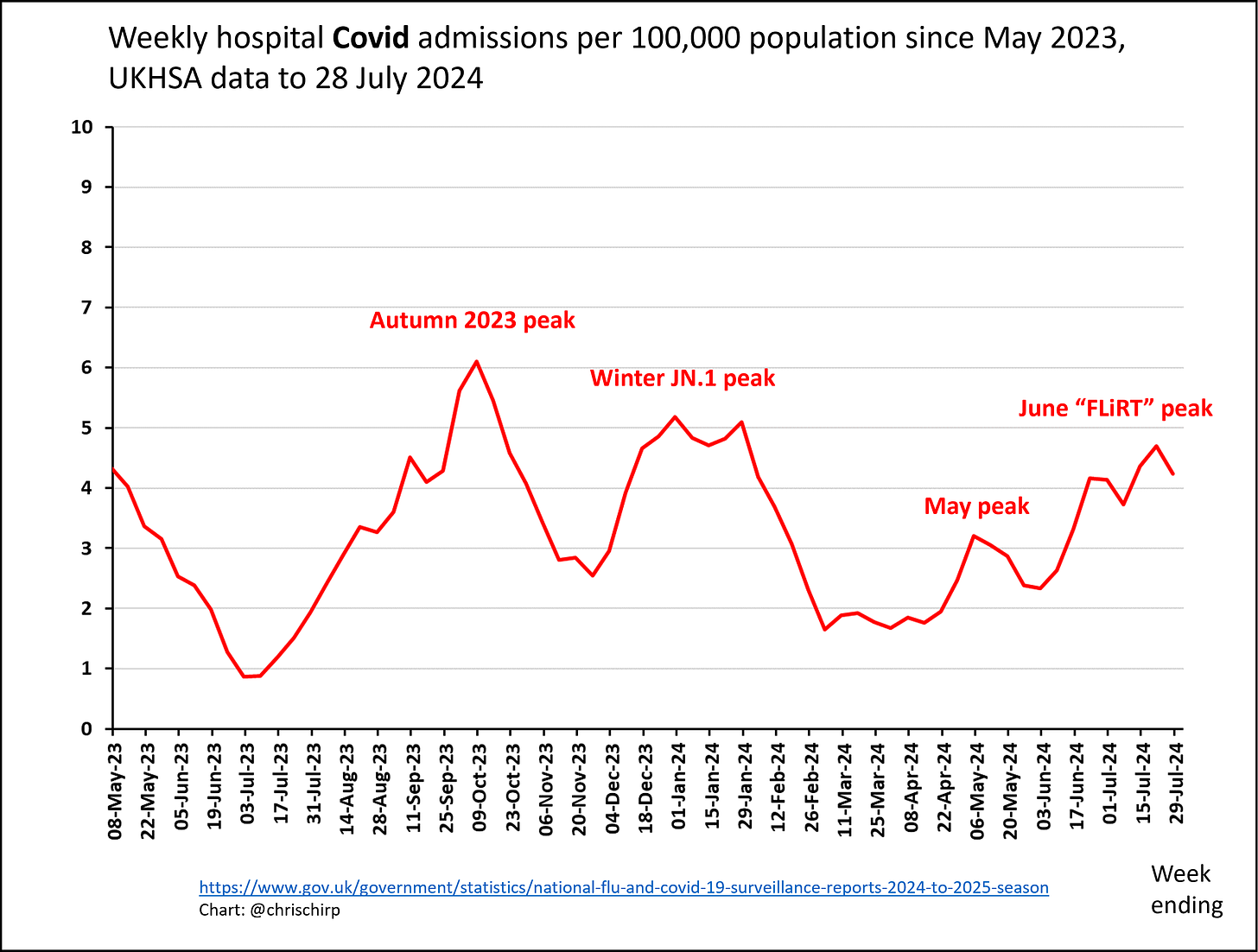
Ideally we want to know prevalence - how many people are infected - not just hsopital admissions. The closest we can get to prevalence in England (and it’s not that close) is wastewater monitoring in Scotland. Wastewater monitoring cannot be directly related to overall prevalence because how much virus is picked up in wastewater depends a lot on individual people’s responses to infection and the variants involved. Basically, some people just shed a lot more virus than others and some variants might make it more likely for virus to be excreted out. All that said, wastewater monitoring is the best we have in the absence of a random infection survey, as it does not depend on testing or being sick enough to need hospital.
Subscribe
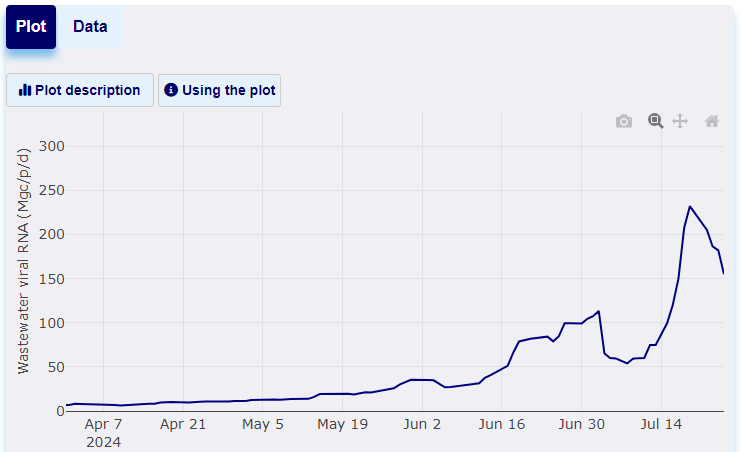
So - what does it show? Well, Scotland shows an enormous July spike - the highest we’ve seen since the first year of Omicron in 2022! Even if there is not an exact correlation with prevalence, I think it is unarguable that Scotland is seeing a very large Covid wave and, very likely, England too. The question is what happens when people return to school and work in September in England and life moves back indoors?
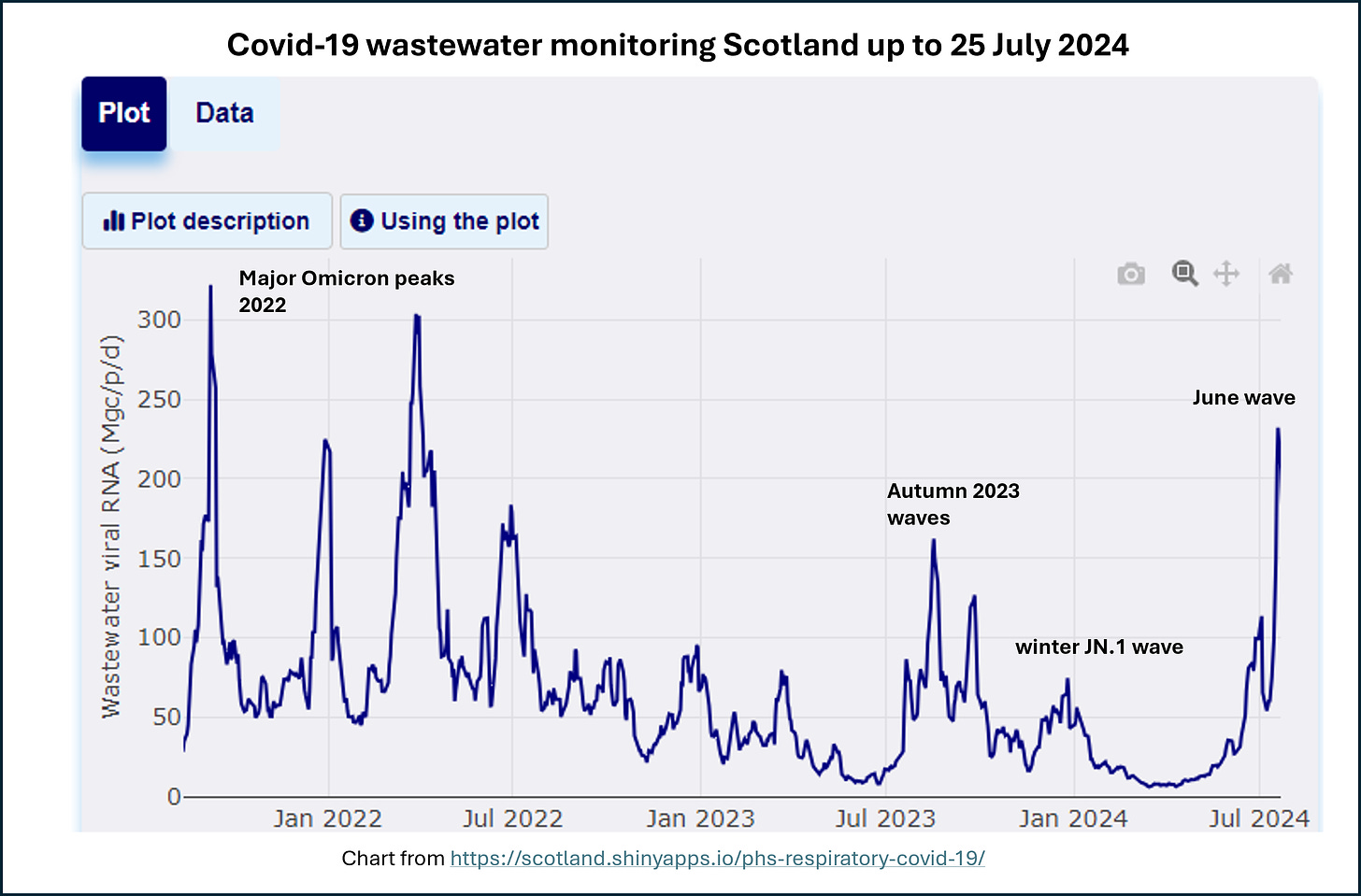
It’s worth noting that Edinburgh Fringe Festival is about to start for the whole of August, and schools go back in Scotland in a few weeks. Both will create excellent conditions for Covid to spread. If you’re going to the festival, please consider wearing a good mask at shows - and if you feel ill or test positive for Covid, then try to avoid contact with others.
The most recent week of the wastewater data does show decline (see below) - but I was too optimistic about the fall in June so I’ll wait for another week or two before being confident of a peak - especially given the festival.
If you feel sick with cold or flu symptoms, it’s probably Covid.
While Covid is going strong, UKHSA reports that other respiratory viruses remain at low levels. There is some rhinovirus circulating (causes a common cold), but honestly, if you have cold or flu symptoms then it most likely to be Covid. If you feel ill, please consider testing and/or restricting your activities until you feel better or test negative. Also, it’s important to rest to further reduce your chances of developing Long Covid.Share
Prof Trish Greenhalgh has just written a brilliant substack summarising the latest research on Long Covid and I’ve snipped a bit below:
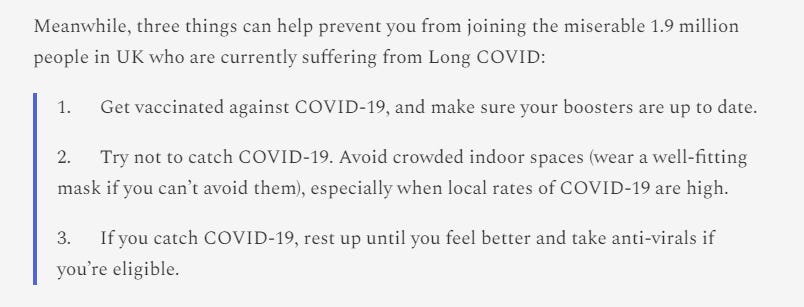
Covid is causing less harm than it did during the pandemic’s height, but it still causes harm and people are getting ill more often than they used to, with consequent disruption to their lives. This is both because we’ve added a new disease to our population and because Covid is stubbornly not seasonal and is still creating several waves a year. Research into broader, longer lasting, Covid vaccines continues - I believe this should be a prioritised research effort so that we can really give the virus a kick in the teeth.
Thanks for reading Diving into Data & Decision
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,538

Cruisers contracting COVID-19 during summer surge as healthcare recommendations change
COVID-19 cases are surging across the country, and Florida is a hotbed for the virus right now. According to the Centers for Disease Control and Prevention, the Sunshine State is one of 21 states recording high levels of cases.
Cruisers contracting COVID-19 during summer surge as healthcare recommendations change
By Esther BowerUpdated July 30, 2024 8:59pm EDT
Brevard County
FOX 35 Orlando
Family see COVID-19 cases after cruise trip
COVID-19 cases are surging nationwide, with Florida emerging as a hotspot for the virus. It is one of 21 states recording "high" levels of cases, according to the Centers for Disease Control and Prevention. Doctors report a decline in hospitalizations for COVID-19, but they are witnessing a spike in summer illnesses. Four years into the pandemic, treatment recommendations have evolved, according to medical professionals.BREVARD COUNTY, Fla. - COVID-19 cases are surging across the country, and Florida is a hotbed for the virus right now.
According to the Centers for Disease Control and Prevention, the Sunshine State is one of 21 states recording high levels of cases.
https://www.googleadservices.com/pa...WxiNsLYbxSsP3zdpeq-WyCJgUEovMj8w8Two_KIATDXBQ
Available AR Heads-Up DisplayKia Canada|
Sponsored
Doctors say they’re not sending as many people with the coronavirus to hospitals anymore, but they are seeing a summer sickness spike. As years passed post-pandemic, so did healthcare providers' recommendations regarding boosters and isolation.
Cruisers have been especially shocked to come down with COVID-19 on their recent trips. Many are sharing stories on social media about entire families getting sick during or right after they left the ship.
Valerie Fletcher is a recent cruiser with COVID now, after just getting off on the Allure of The Seas.
She and dozens of her family members were on board as part of an 80-person family reunion.
"Every day, someone is reporting they have COVID," said Fletcher, who says this is her first time getting COVID. "There are like 20 of us who have COVID."
She’s not alone. Cases are up nationwide and in Florida.
MORE HEADLINES:
- Ocala laundromat explosion leaves 4 injured, firefighters say
- Florida dad abandons daughter, 10, on 'dangerous' Kissimmee road after late-night spat: sheriff
- Orlando man arrested for sexually battering woman at UCF Downtown parking garage, police say
"The cases are definitely rising," said Dr. Michael Sparks, a primary care physician with Sparks Family Medicine in Sanford.
He says COVID’s changed over the last four years, and so have recommendations from healthcare providers.
"The reality is, COVID is very different than it was a few years ago," said Sparks.
If one tests positive for COVID-19, Dr. Sparks recommends delaying a return to work until one goes "24 hours without a fever and is not on fever-reducing meds."
When asked about vaccines and boosters, Dr. Sparks replied, "That’s tricky," and added, "There’s this question of risk versus benefit that comes up. For a lot of people, that’s an individual question at this point."
The symptoms for most people right now are similar to the flu and having a cold.
"It was body aches and then just stuffiness in my head. I feel like I have a head cold," said Fletcher.
She's staying home and taking over-the-counter meds for now as she recovers from her cruise that ended with COVID-19.
"Next time, I’m taking my mask and wearing it on the elevators," concluded the cruiser.
Dr. Sparks says not all of his patients are testing for COVID anymore. The tests aren’t free, so that’s changed things for people.
He recommends testing if you are in contact with someone with a weaker immune system or a senior citizen. Certain populations can still be severely affected by the disease, and it’s good to know if you are positive for COVID-19 and around those people.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,539

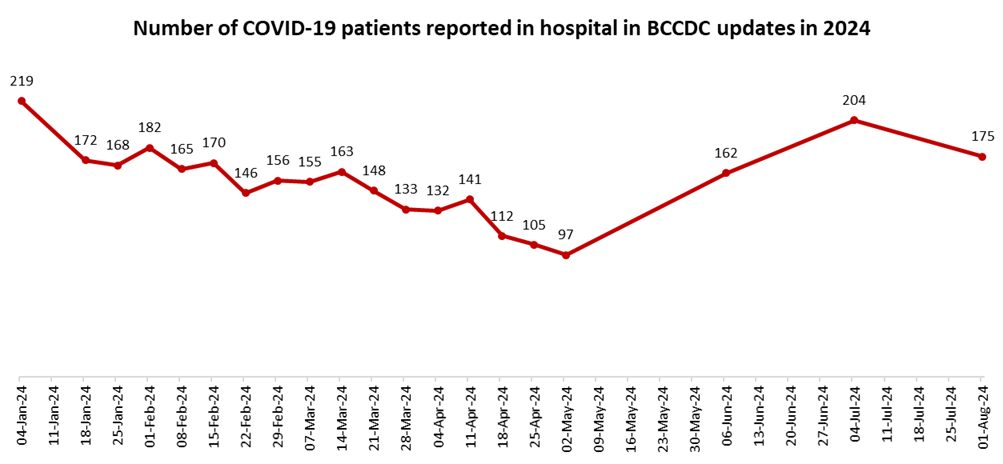
175 in hospital with COVID-19 in BCCDC's first update since end of public health emergency
The first COVID-19 data released by the B.C. Centre for Disease Control since the official end of the province's public health emergency shows hospitalizations decreasing, but still near their highs for the year.
175 in hospital with COVID-19 in BCCDC's first update since end of public health emergency

Ian Holliday
CTVNewsVancouver.ca Reporter
Contact
Published Aug. 1, 2024 9:01 p.m. EDT
The first COVID-19 data released by the B.C. Centre for Disease Control since the official end of the province's public health emergency shows hospitalizations decreasing, but still near their highs for the year.
There were 175 test-positive COVID patients in B.C. hospitals as of Thursday, according to the BCCDC. That's down from 204 at the start of last month, but still the fourth-highest total of 2024, and more than double the 76 people hospitalized at this time last year.
Last week, provincial health officer Dr. Bonnie Henry announced she was ending the COVID-related public health emergency declaration that had been in place since early 2020.
The move meant all remaining restrictions – principally the vaccine mandate that remained in place for most health-care workers – would be lifted, and unvaccinated health-care workers could reapply for jobs in B.C.'s health system.
Critics panned the move as both too late and politically motivated, noting that B.C. was the last province in Canada to end its vaccination requirement, has been struggling to keep emergency departments in rural areas open due to staff shortages, and has a provincial election upcoming in October.
Henry and Health Minister Adrian Dix defended the move, saying the vaccine mandate was "instrumental" in protecting health-care workers and patients, and that the number of workers fired for refusing the vaccine was relatively small.
The provincial health officer added that the decision to end the public health emergency had "nothing to do" with the election.
"There is an obligation under the Public Health Act for me to lift orders as soon as reasonably possible when the conditions are no longer met," Henry said.
She added that the change could potentially have been made "a few months ago," but there was still uncertainty around the impacts of a spring wave of COVID-19.
Indeed, Henry noted that uncertainty around the coronavirus that shut down the world back in 2020 remains, and said transmission would likely surge again in the fall.
"We know (the virus) is inevitably going to mutate," she said. "It may be that we'll need to have different varieties of the vaccine over time."
Henry characterized the number of people ending up in hospitals and intensive care units because of COVID-19 as "lower and stable," and CTV News tracking of BCCDC data supports this conclusion.
The highest hospitalization total seen in the province in 2024 so far is 219, and all but two published updates have shown totals below 200.
In 2023, the number of people in hospital with COVID varied more widely, from as high as 422 to as low as 76.
In 2022, the published total climbed as high as 1,054 in the early days of the Omicron variant, and the lowest total recorded for the year was 255.
The BCCDC's most recent update showed 368 new, lab-confirmed COVID infections in the province, though that number significantly underestimates the spread of the virus because most people in the province do not qualify for lab-based testing.
Wastewater surveillance data(opens in a new tab), which is published weekly and can help approximate the prevalence of COVID in the broader community, has shown "elevated" concentrations of the virus for the last several weeks, but is "stabilizing or decreasing" in most locations, according to the BCCDC.
With files from The Canadian Press
Last edited:
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,540
Nasal COVID-19 vaccine halts transmission | Washington University School of Medicine in St. Louis
Study in hamsters indicates vaccines targeting nose, mouth may be key to controlling spread of respiratory infections
 medicine.wustl.edu
medicine.wustl.edu
Nasal COVID-19 vaccine halts transmission
Study in hamsters indicates vaccines targeting nose, mouth may be key to controlling spread of respiratory infectionsby Tamara Schneider•July 31, 2024
A nasal COVID-19 vaccine blocks transmission of the virus, according to an animal study by researchers at Washington University School of Medicine in St. Louis. The findings suggest that vaccines delivered directly to the nose or mouth could play a critical role in containing the spread of respiratory infections.
The lightning-fast development of COVID-19 vaccines just months after the virus appeared was a triumph of modern science and saved millions of lives. But for all the good they did in reducing illnesses and deaths, the shots were unable to end the pandemic because of one notable weakness: They couldn’t stop the spread of the virus.
A new study by researchers at Washington University School of Medicine in St. Louis indicates that next-generation vaccines that target the virus’s points of entry — the nose and mouth — may be able to do what traditional shots cannot: contain the spread of respiratory infections and prevent transmission. Using a nasal COVID-19 vaccine based on Washington University technology, approved for use in India and licensed to Ocugen for further development in the U.S., the researchers showed that vaccinated hamsters that developed infections did not pass the virus on to others, breaking the cycle of transmission. In contrast, an approved COVID-19 vaccine that is injected failed to prevent the spread of the virus.
The findings, published July 31 in Science Advances, provide further evidence that so-called mucosal vaccines sprayed into the nose or dropped into the mouth may be the key to controlling respiratory infections such as influenza and COVID-19 that continue to circulate and cause significant illness and death.
“To prevent transmission, you need to keep the amount of virus in the upper airways low,” said senior author Jacco Boon, PhD, a professor of medicine, of molecular microbiology and of pathology & immunology. “The less virus that is there to begin with, the less likely you are to infect someone else if you cough or sneeze or even just breathe on them. This study shows that mucosal vaccines are superior to injected vaccines in terms of limiting viral replication in the upper airways and preventing spread to the next individual. In an epidemic or pandemic situation, this is the kind of vaccine you’re going to want.”
Developing vaccines that can control virus levels in the nose has proven challenging. Viruses such as influenza virus, SARS-CoV-2 (the virus that causes COVID-19) and respiratory syncytial virus (RSV) multiply rapidly in the nose and spread from person to person within a few days of initial exposure. Traditional injectable vaccines generate immune responses that can take a week to build to full strength and are much less potent in the nose than in the bloodstream, leaving the nose relatively unprotected against a fast-multiplying, fast-spreading virus.
In principle, a vaccine sprayed or dropped directly into the nose or mouth could limit viral reproduction and thereby reduce transmission by eliciting an immune response right where it’s needed most. But gathering evidence that mucosal vaccines actually do reduce transmission has proven tricky. Animal models of transmission are not well-established, and tracking person-to-person transmission is fiendishly complicated, given the number and variety of encounters a typical person has on any given day.
For this study, Boon and colleagues developed and validated a model for community transmission using hamsters and then used it to assess the effect of mucosal vaccination on the spread of SARS-CoV-2. (Unlike mice, hamsters are naturally susceptible to infection with SARS-CoV-2, making them the ideal laboratory animals for a transmission study.)
The researchers immunized groups of hamsters with laboratory versions of approved COVID-19 vaccines: the nasal iNCOVACC used in India or the injected Pfizer vaccine. For comparison, some hamsters were not immunized. After giving the vaccinated hamsters a few weeks for their immune responses to fully mature, the researchers infected other hamsters with SARS-CoV-2 and then placed the immunized hamsters with the infected hamsters for eight hours. This first step of the experiment mimics the experience of vaccinated people who are exposed to a person with COVID-19.
After spending eight hours rubbing shoulders with infected hamsters, most of the vaccinated animals became infected. Virus was found in the noses and lungs of 12 of 14 (86%) hamsters that had received the nasal vaccine, and 15 of 16 (94%) hamsters that had received the injected vaccine. Importantly, while most animals in both groups were infected, they weren’t infected to the same degree. Hamsters that had been nasally immunized had virus levels in the airways 100 to 100,000 times lower than those that had received the shot or had not been vaccinated. The study did not assess the animals’ health, but previous studies have shown that both vaccines reduce the likelihood of severe illness and death from COVID-19.
The second step of the experiment yielded even more striking results. The researchers took vaccinated hamsters that subsequently developed infections and placed them with healthy vaccinated and unvaccinated hamsters for eight hours to model transmission of virus from a vaccinated person to others.
None of the hamsters that were exposed to nasally vaccinated hamsters became infected, regardless of whether the recipient hamster had been vaccinated or not. In contrast, roughly half of the hamsters that were exposed to hamsters vaccinated by injection became infected — again, regardless of the recipient’s immunization status. In other words, vaccination through the nose — but not by injection — broke the cycle of transmission.
These data, Boon said, could be important as the world prepares for the possibility that avian influenza, currently causing an outbreak in dairy cows, might adapt to humans and trigger a flu epidemic. An injectable vaccine for avian influenza already exists, and a team of researchers at Washington University is working toward a nasal vaccine for avian influenza. That team includes Boon and co-author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine and one of the inventors of the nasal vaccine technology used in this paper.
“Mucosal vaccines are the future of vaccines for respiratory infections,” Boon said. “Historically, developing such vaccines has been challenging. There’s still so much we don’t know about the kind of immune response we need and how to elicit it. I think we’re going to see a lot of very exciting research in the next few years that could lead to big improvements in vaccines for respiratory infections.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,541

Moderna’s Future Clouded With Vaccines Facing New Pressures
Moderna Inc.’s post-pandemic future was thrown into question Thursday after it disclosed multiple setbacks that disappointed investors.
Moderna’s Future Clouded With Vaccines Facing New Pressures
By Gerry SmithAugust 01, 2024 at 4:12PM EDT

A researcher in a lab at the Moderna Inc. headquarters in Cambridge, Photographer: Adam Glanzman/Bloomberg (Adam Glanzman/Bloomberg)
(Bloomberg) -- Moderna Inc.’s post-pandemic future was thrown into question Thursday after it disclosed multiple setbacks that disappointed investors.
The biotech company has been largely shut out of the Covid vaccine market in Europe and expects low sales there. It’s facing increased competitive pressure in the US, leading to a disappointing launch of its new RSV vaccine.
The obstacles prompted the company to reduce its sales expectations for the year. The shares fell a record 21% on Thursday, erasing their 2024 gains.
The Cambridge, Massachusetts-based company is trying to manage the decline of its Covid vaccine business as it spends billions to develop new uses for mRNA technology. While Moderna has added an RSV vaccine to its portfolio, how soon investors can expect additional products that could boost sales — including a flu shot and highly-anticipated cancer vaccine — remains unclear.
Despite cost cuts, Moderna posted a second straight quarterly loss. It now sees 2024 sales ranging between $3 billion and $3.5 billion, down from its previous outlook of about $4 billion, according to a second-quarter earnings statement. The company has said it doesn’t expect to break even until 2026.
The forecast cut “heightens concerns, given Moderna is already running net losses and raises doubt about hitting profitability and cash burn goals,” Jefferies analyst Michael Yee said in a note.
Revenue for the quarter was $241 million. While that’s down about 30% from the same period a year ago, it surpassed analysts’ expectations. The company gets the bulk of its sales in the second half of the year when people seek Covid shots to prepare for the colder months and the rise of most respiratory infections.
What Bloomberg Intelligence Says:
Moderna’s reduced 2024 sales guidance of $3-$3.5 billion, from $4 billion at the end of 1Q, may still not be enough, given vaccine fatigue and the competitive nature of the nascent US market. The lack of any commentary on the potential sales of its mRESVIA RSV vaccine is also a concern.
— BI analyst Sam Fazeli. Read the research here.
Moderna Chief Financial Officer James Mock attributed the sharp year-on-year sales decline to the fact that some 2022 vaccine orders were included in last year’s figures. The quarter’s sales beat expectations because more people are getting immunized than had been anticipated, he said.
“There’s been a steady amount of vaccinations that was more than we had assumed in our revenue guidance,” he said in an interview.
‘Very Low’
Moderna has been in discussions to sell its Covid shot in Europe, where Pfizer Inc. and its partner, BioNTech SE, already have a deal in place. Based on recent discussions, Moderna said it now expects “very low” sales in the region. The company also cut its revenue guidance for the year because some international sales are tied to vaccination rates and may be deferred to next year, according to Mock.
After the May US approval of its RSV vaccine in older adults, Moderna began deliveries in July. But new data presented in June showed the efficacy of Moderna’s shot fell sharply over time and was lower than rival vaccines.
The results could raise doubts over how much the product will financially benefit Moderna, which was third to the market after Pfizer and GSK Plc introduced vaccines last year for RSV, an illness that affects elderly adults and babies most severely.
On the earnings call, Mock said Moderna’s RSV launch this year is “not turning out as we expected,” in part because competitors had already negotiated some contracts. Moderna is hoping to capture a “more fair market share” in 2025, Mock said.
The company is investigating other ways to develop or use the mRNA technology that underpins its Covid vaccine. In July, Moderna secured nearly $200 million from the US government to speed development of an mRNA vaccine for pandemic influenza as a dangerous strain of bird flu sweeps through US dairy farms.
(Updates with shares in third paragraph.)
©2024 Bloomberg L.P.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,542
:max_bytes(150000):strip_icc()/Health-GettyImages-1340281386-96327461363f4af2bccc1bc326dd4db0.jpg)
The Science Behind Why COVID-19 Tends to Spike During Summer Months
The U.S. is in the middle of another COVID-19 "summer surge" as "high" or "very high" levels of the virus have been detected across most of the country. COVID tends to spike during the summer months due to rising temperatures, more gatherings, and an evolving virus.
The Science Behind Why COVID-19 Tends to Spike During Summer Months
ByElizabeth Yuko, PhD
Fact checked by
Nick Blackmer
:max_bytes(150000):strip_icc():format(webp)/untitled-5582-Edit-d19315b04e5a4b7e85ec15100d87de46.jpg)
Fact checked byNick Blackmer
Nick Blackmer is a librarian, fact-checker, and researcher with more than 20 years of experience in consumer-facing health and wellness content.
health's fact checking process
0 of 34 secondsVolume 0%
Are You Eating Too Many Potatoes?
Close
- The U.S. is in the middle of another COVID-19 "summer surge."
- "High" or "very high" levels of the virus have been detected across most of the country.
- COVID tends to spike during the summer months due to rising temperatures, more gatherings, and an evolving virus.
According to wastewater surveillance data from the Centers for Disease Control and Prevention (CDC), “high” levels of the virus have been detected across much of the country, with the exception of 19 states—primarily in the western parts of the U.S.—where levels are “very high.”2
While inconvenient, it’s normal for COVID to spike in the summer months—in fact, summer surges have happened every summer since COVID arrived on the scene. Here’s what to know about this increase in cases, including why it tends to happen during summertime, and how to protect yourself from the virus.
:max_bytes(150000):strip_icc():format(webp)/Health-GettyImages-1340281386-96327461363f4af2bccc1bc326dd4db0.jpg)
izusek / Getty Images
What Is a Summer Surge?
A COVID summer surge is “when there’s an unexpected increase in the number of COVID cases” during the summer months, according to Nikhil Bhayani, MD, an infectious disease physician and assistant professor at Burnett School of Medicine at Texas Christian University.Other than allergies, we tend to associate mild infectious illnesses like the cold, flu, and now COVID with fall and winter. But technically, those viruses can surge any time of the year, said Bhayani.
“We see a surge in summer because people are traveling more, gathering frequently indoors and not masking as much,” he told Health. “The virus evolves and stays ahead of our immune system. As new variants appear, the immune system recognizes infection of past variants—so this can lead to an increase in new infections.”
Vontrelle Roundtree, MD, board-certified family physician and associate chief medical officer at MDLIVE, said that the telehealth clinic has “seen a steep surge in COVID-19 cases since the beginning of the summer,” with diagnoses up 108%. Paxlovid prescriptions also increased 130% in June over the monthly average for April and May.
How To Tell If You Have a Summer Cold or COVID
What’s Behind the Current Summer Surge?
There are several reasons why COVID cases have been on the rise this summer and during previous summers. The first is that many people don’t currently have immunity to the virus. “Immunity to prior COVID infection is short lived,” said Bhayani, adding that it tends to “wane after three months.”In other words, if you’re relying on your immunity to protect you against COVID, you’re going to need a new strategy—like getting vaccinated. “Vaccinations are effective in maintaining immunity for a relatively longer period of time,” he said.
Not only that, but the FLiRT COVID variants are largely driving this surge and “may be more adept at evading the immune system,” Roundtree said. “They’re offshoots of the JN.1 variant which we saw earlier this year,” she added.
The weather might also play a role in the summer surge. According to Bhayani, some of the emerging variants might thrive more in the heat than the cold, so “we could see a little more of an increase in COVID than the late fall or early winter.” Additionally, the extreme heat in many parts of the country is “driv[ing] more people to gather together in indoor settings,” Roundtree added.
Along the same lines, increased summertime social activities, events, and travel “set the stage for a significant rise in cases and complicates any existing efforts to manage the spread,” Roundtree said. This includes people getting together to watch the Summer Olympics.
“It’s certainly possible that the Summer Games may cause an uptick in COVID-19 cases,” Roundtree said. “Large gatherings of any kind create an optimal environment for the virus to spread easily, regardless of whether they take place outside or indoors.”
This is true for people having guests over to their homes to watch the Olympics on TV, as well as those attending the games in person in Paris. “With athletes and spectators traveling from all different parts of the world, the risk of transmission increases significantly,” she explained. “In fact, we’ve already seen some attendees and athletes testing positive over the last few days.”
Will COVID Continue to Surge?
According to Bhayani, COVID will continue to surge this summer “as long as people travel and gather indoors.” But Roundtree is hopeful that we won’t see another surge until late fall or early winter when people travel and get together for the holidays. That said, if people take precautions, another spike in cases isn’t guaranteed. “When a new vaccine is available in early fall, and people choose to get vaccinated, maybe the surge won’t be as high compared to summer months,” she said.How to Protect Yourself During COVID Surges
To prepare for a summer surge and reduce your chances of contracting COVID during the summer, Bhayani and Roundtree recommend the following:- Wearing a mask in crowded spaces both outdoors and indoors—especially if you or a loved one has a compromised immune system
- Staying up-to-date on vaccinations and boosters
- Testing for COVID regularly
- Practicing good hygiene by regularly washing your hands and using hand sanitizer
- Opening windows
- Using HEPA air filtration to reduce the risk of transmission
“If you experience symptoms such as a sore throat, cough, fatigue or muscle aches, be sure to get tested and see your provider for treatment options,” Roundtree said. “As we approach the fall season, it’s especially important to consult with a physician who can help distinguish between COVID-19 and other respiratory infections like the flu or colds, as symptoms are often similar.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,543
Some Olympians test positive for COVID, but it's business as usual for many athletes
More than 12 Olympic athletes have reportedly tested positive for COVID-19 in Paris

Kiera Osborne · CBC News · Posted: Aug 02, 2024 4:00 AM EDT | Last Updated: 3 hours ago

Coaches from the Netherlands wear face masks during the 2024 Paris Olympics on July 31. More than a dozen athletes have tested positive for COVID-19 so far in Paris, where Olympic rules and protocols are more relaxed than they were during the Tokyo Games that were held in 2021 at the height of the pandemic. (Oli Scarff/AFP/Getty Images)
Social Sharing
- X
But COVID's impact seems to have dropped significantly since Tokyo.
The Paris Olympics continue to operate normally — spectators gather in the stands, and athletes congregate freely at mealtime.
But a closer look shows masks are slowly popping up on athletes, and a few faces are missing from the start lines.
Some athletes compete, others withdraw
More than a dozen athletes in Paris have reportedly tested positive for COVID-19, including British swimmer Adam Peaty, who tested positive on Sunday evening after winning silver in the 100m breaststroke, the Guardian reported Tuesday.Another swimmer, Australia's Lani Pallister, withdrew from the 1500m freestyle on Tuesday after a positive COVID test.

From left, Team Australia gold medallists Mollie O’Callaghan, Lani Pallister, Brianna Throssell and Ariarne Titmus pose on the podium after the women's 4x200m freestyle relay final on Aug. 1. Pallister withdrew from another event on Tuesday after testing positive for COVID-19. (Adam Pretty/Getty Images)
Since athletes who test positive are still allowed to compete in Paris, it was decided that Pallister would rest and prepare for the 4x200m freestyle, according to the Australian Olympic Committee. That decision paid off when the team won gold in the event on Thursday.
But another athlete's 2024 Olympic dreams were crushed altogether.
German decathlete Manuel Eitel made a statement on Instagram about withdrawing from the Paris Olympics due to a COVID infection.
"Today is and will be one of the worst days of my life," he said in a post written in German.
"How many times I've fought, how hard I've worked to earn these games, few people know."

German decathlete Manuel Eitel recently announced on his social media that he was withdrawing from the Paris Games due to COVID. (David Ramos/Getty Images)
Rules and protocols in Paris
There are limited protocols and restrictions in place at the Olympics, Reuters reported on Tuesday."We have a protocol [that] any athlete that has tested positive has to wear a mask, and we remind everyone to follow best practices," said Anne Descamps, Paris 2024 chief communications director.
Beyond those protocols, individual athletes and their countries have been left to make their own decisions about preventing and dealing with the virus.
What coronavirus variant is causing most infections in Canada these days and what are the symptoms?
Some countries have taken COVID prevention into their own hands.
Team Great Britain has been seen wearing masks between events, and Canada has continued to implement pandemic-era protocols including hand washing and sanitation, Reuters reported. Canada's chief medical officer Mike Wilkinson said they also have isolation protocols for anyone who does get sick.
For athletes that have tested positive, the decision about whether to compete can be a complex one, said Dr. Alexandra Rendely, a staff physician in physical medicine and rehabilitation at the University Health Network's (UHN) Toronto Rehabilitation Institute.
"It's going to be up to each individual competitor and their medical staff for that country to determine if the symptoms they have are compatible with allowing them to compete, both at their highest degree of competition, but also from a safety standpoint," she said.
Rendely gave the example of a swimmer, where shortness of breath or a cough, both symptoms of COVID, can change an athlete's breathing patterns. She also noted that these symptoms, along with muscle aches and fever, can change the speed at which athletes use their arms and legs.
Tokyo's strict approach
The previous games were completely transformed from the status quo.After the Tokyo Games were delayed a year due to the pandemic, strict regulations banned spectators from attending, and any athlete that tested positive had to immediately self-isolate and was not allowed to compete.
Masking, social distancing and regular testing were also required.
Some members of Canada’s Olympic delegation were placed under COVID-19 protocols upon arrival in Beijing. These protocols are strict — with Chinese officials hoping to keep COVID-19 out of the Olympics just days before it begins.
"For good reason, COVID is less on our radar than it was two years ago, three years ago," said Dr. Alon Vaisman, an infectious diseases and infection control physician at UHN.
Vaisman said both the virus and what we know about treating it have changed.
While some athletes might be able to physically compete while infected with COVID, the question remains: should they?
Many Olympic events involve close contact with other people, meaning there's an increased risk of transmission between athletes. Vaisman says athletes shouldn't be taking part in events while experiencing symptoms like a cough or runny nose.
"That's more like a moral responsibility, more than anything," he said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,544
Masking returns to Guelph General Hospital following COVID-19 outbreak
Hospital brings back masking with the guidance of Wellington-Dufferin-Guelph Public Health
Lauren Kuivenhoven · CBC News · Posted: Aug 02, 2024 12:06 PM EDT | Last Updated: 2 hours ago

Masking is required again in clinical areas of Guelph General Hospital as of this week. (Paula Duhatschek/CBC)
Social Sharing
- X
It's a precautionary step to prevent further cases, Karen Suk-Patrick, the hospital's vice-president, said in a news release.
The new masking rules follow a rise in COVID-19 cases throughout the community and hospital.
Masks are required in clinical areas of the hospital, such as nursing stations, patient rooms and waiting rooms. Since the requirements are in the first phase, masks are not required in non-clinical areas.
The hospital has masking stations at entrances and nursing stations.
Summer weather meant decreasing COVID-19 numbers, but the cases were never at zero, said Dr. Matthew Tenenbaum, the Wellington-Dufferin-Guelph Public Health associate medical officer.
"It's still one of the things out there in the environment."
Wearing a mask is a valid practice any time of the year, said Tenenbaum. He said it's also recommended to wear one when feeling cold and flu symptoms.
Users who are viewing this thread
Total: 2 (members: 0, guests: 2)
Pakistan Defence Latest
-
-
Israel and USA 'jammed GPS signals' in days before Iran's 300-missile launch to confuse attackers (9 Viewers)
- Latest: Cash gk
-
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (3 Viewers)
- Latest: Cookie Monster
-
Country Watch Latest
-
-
Will the UAE reconsider the deal to purchase F-35 fighters with Trump’s possible return? (3 Viewers)
- Latest: harpy1
-
-
-
Latest Posts
-
-
-
-
Will the UAE reconsider the deal to purchase F-35 fighters with Trump’s possible return? (3 Viewers)
- Latest: harpy1
-
