Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,772

11 Top COVID Symptoms People Are Experiencing During the Summer Surge
There are several COVID variants, some strains are being referred to as FLiRT, while another is LB.1. Here are the COVID symptoms to watch out for this summer.
11 Top COVID Symptoms People Are Experiencing During the Summer Surge
Irina GonzalezTue, August 13, 2024 at 9:20 AM EDT·6 min read
Scroll back up to restore default view.
- There are several COVID variants right now which have the same "set of mutations," and are being referred to as FLiRT. Another strain, LB.1, is also on the rise.
- KP.3.1.1 — which comes from the JN.1 strain — is now the most dominant variant, accounting for an estimated 27.8% of cases.
- The symptoms are similar to other COVID strains. Being sick and experiencing a chronic cough, elevated fever, sore throat or a runny nose should prompt you to get a COVID-19 test to ensure you are not contagious.
If it seems like more people around you have gotten COVID in the last couple of months, that's probably true. Right now, cases are on the rise and the COVID-19 FLiRT variants are dominating.
According to the most recent estimates from the Centers for Disease Control and Prevention (CDC) released on August 3rd, 27.8% of cases are the KP.3.1.1 strain and 20.1% of current infections are KP.3. Both of these variants stem from the FLiRT family of the coronavirus. Another variant that is not a descendant of FLiRT, named LB.1, makes up an estimated 16% of COVID-19 cases at the moment.
“The FLiRT variant appeared in March,” says Tammy Lundstrom, M.D., J.D., the senior vice president at Trinity Health who led their COVID-19 response. “Throughout the COVID-19 era, new strains have continued to arise. Like other strains, it appears highly transmissible, but it does not appear more virulent at this point.”
While it's great that COVID-19 cases don't seem to be as dangerous as they used to be, it still causes unpleasant symptoms which can be severe for people with certain risk factors. Unfortunately, just 22.5% of American adults had received the most recent COVID-19 vaccine as of May 11, 2024 (when the latest data was released). Could this be contributing to the summer surge we're experiencing? We turned to experts to learn more about the newest variants, important COVID-19 symptoms to be aware of and how to protect yourself and your loved ones.
What are the FLiRT and LB.1 variants?
As fun as the name sounds, FLiRT is not the official designation for the dominant COVID-19 variant. That is actually a cheeky nickname for a whole family of different variants (any that start with KP). “The FLiRT variants came to the forefront at the end of April,” says Nikhil K. Bhayani, M.D., FIDSA, an infectious disease specialist and assistant professor at the Burnett School of Medicine at Texas Christian University.KP.2, KP.2.3, KP.3 and KP.3.1.1 are official names of the FLiRT variants that are circulating right now. While FLiRT took over JN.1 as the dominant variant, it's actually a descendant of JN.1. Essentially, the “parent” variant (JN.1) was unseated by several “child” variants. Various variations of JN.1 are still swirling in some capacity, but they make up a smaller percentage of COVID-19 cases. LB.1, another variant that has been circulating this summer, is not a member of the FLiRT family, but another descendant of JN.1.
Is there a summer surge?
Yes, the wastewater viral activity for COVID-19 — how the CDC tracks trends in infectious disease circulating in a community — is currently listed as “very high,” according to the most recent CDC data. However, a summer surge is not unique to FLiRT.“Throughout the COVID-19 era, we have seen a rise in infections during summer,” says Dr. Lundstrom. Two reasons for this, according to the CDC, are that people tend to do more traveling during the summer and also congregate indoors with air conditioners on when it's very hot outside.
What are the symptoms?
The good news is that the FLiRT and LB.1 strains of the coronavirus don’t seem to spark any surprise symptoms. “The symptoms are similar to other COVID-19 strains,” says Dr. Lundstrom. The CDC updated its list of possible symptoms on June 25th, and those include:- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Sore throat
- Congestion or runny nose
- New loss of taste or smell
- Fatigue
- Muscle or body aches
- Headache
- Nausea or vomiting
- Diarrhea
How long do symptoms last?
It really depends on the person. Typically, people with mild cases will experience symptoms for 5-10 days, however, many may start to feel better sooner than that. According to the CDC, most people with long COVID will start to feel better after three months, although it can last years. It's best to speak to your doctor if any of your symptoms are lingering.Is there a new vaccine?
Our experts said that vaccines still provide good protection against COVID-19, “especially against severe illness and hospitalization,” says Dr. Lundstrom. However, a study published in April found that KP.2 is proving to have “the most significant resistance” to the 2023-24 COVID-19 booster, and that this “increased immune resistance ability of KP.2 partially contributes to the higher” prevalence of infections “than previous variants, including JN.1.”At the end of June, the CDC recommended that everyone ages 6 months and older receive the updated 2024-25 COVID-19 vaccine, which was tweaked based on the most dominant variants circulating this year. The most updated COVID-19 vaccine is expected to be rolled out this fall. “The World Health Organization is recommending the upcoming COVID booster to be based on the predominant lineage for the year,” adds Dr. Bhayani.
However, the CDC and our experts still recommend the current vaccine to protect yourself before the 2024-25 booster is made available in the fall. “Adults over the age of 65 should get the last COVID-19 vaccine available,” says Bhayani. Dr. Lundstrom suggests that older adults “should be vaccinated four months after their last vaccination” and those with compromised immune systems “should get vaccinated two months after their last dose.”
How to protect yourself
In March, the CDC updated the Respiratory Virus Guidance as COVID-19 cases have decreased over time. “It is still an important health threat, but it is no longer the emergency that it once was, and its health impacts increasingly resemble those of other respiratory viral illnesses, including flu and RSV,” the new guidance states.“The same precautions will help protect against the spread of most respiratory viruses: wash hands frequently, cover your mouth and nose when sneezing/coughing, stay up to date with vaccinations and stay home when ill to prevent spreading infection to others,” suggests Dr. Lundstrom. However, Dr. Bhayani reminds us that the elderly, individuals with compromised immune systems and kids “should take extra precautions, such as avoiding large crowds and wear masks if COVID-19 cases are on the rise locally.”
If you do get sick, the CDC still recommends staying at home until your symptoms are improving overall, and you have not had a fever (and are not using fever-reducing medication). Afterward, you can resume normal activities and “use added prevention strategies over the next five days.”
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,773

Salmon oil playing key role in Covid recovery, say researchers - Fish Farmer Magazine
A medicinal oil product derived from salmon trimmings could play a big part in helping patients to recover from Covid-19. Hofseth BioCare a leader in science- led marine nutrition has announced compelling new findings from a recent study on the benefits of its enzymatically liberated salmon oil...
www.fishfarmermagazine.com
Salmon oil playing key role in Covid recovery, say researchers
August 15, 2024 | Vince McDonagh | News, News Archive, News ArchiveShare on Facebook
Share on Email
Share on Messenger
Share on Linkedin
Share on Pocket
Share on Telegram
𝕏Share on Twitter
Share on WhatsApp

A medicinal oil product derived from salmon trimmings could play a big part in helping patients to recover from Covid-19.
Hofseth BioCare a leader in science- led marine nutrition has announced compelling new findings from a recent study on the benefits of its enzymatically liberated salmon oil (OmeGo), in helping Covid-19 recovery.
Published in the International Journal of Molecular Sciences, this pioneering research has demonstrated that OmeGo has the potential to improve immune responses and reduce inflammation in individuals with mild to moderate Covid-19 infection, caused by the SARS-CoV-2 virus.
The study found that those taking OmeGo had significantly lower levels of pro-inflammatory cytokines, which is vital for reducing the acute inflammatory response linked to the complications of Covid-19.
Additionally, OmeGo supplementation led to better interferon-related gene expression, essential for effective viral clearance and maintaining a balanced immune response.
Hofseth Biocare also said that participants also showed improved lung barrier function and enhanced immune memory, indicating a strong and lasting immune defence.
The company describes OmeGo as an “enzymatically liberated” oil, an approach which means that valuable components of the salmon oil, which is derived from fish off-cuts, are not lost during processing.
For most people, covid-19 is a mild illness that passes, but some suffer from symptoms that last beyond the acute phase.
People who have symptoms that affect functioning in daily life and have lasted for at least two months, are diagnosed with “late sequelae of covid-19”. The diagnosis is usually made three months after the patient has gone through the illness.
Such late effects have also been reported after many other infections, and it is therefore not surprising that some people experience long-term problems after Covid. Covid is a condition affecting an estimated 65 million people globally.
Hofseth believes the research sheds light on the potential role of whole salmon oil in managing long
Dr Crawford Currie, lead author and Head of Medical R&D at Hofseth Biocare said: “The Covid-19 pandemic cast immune health under the spotlight and since then, consumers worldwide have been exploring solutions to proactively boost their viral defences. T
The broad-spectrum benefits of our enzymatically liberated salmon oil stand as a beacon of hope, with this latest study demonstrating its power to modulate the immune response, aid recovery and reduce the risk of severe outcomes. OmeGo® encapsulates the essence of whole fish, offering profound health benefits that extend beyond nutrition to help fortify our immune systems and support recovery from viral infections.”
OmeGo is derived from Norwegian Atlantic salmon and mirrors the lipid profile of whole salmon. It provides unique anti-inflammatory and anti-allergic benefits distinct from omega-3 alone.
Hofseth BioCare’s headquarters are in Ålesund, Norway with branches in Oslo, Chicago, Mumbai, Tokyo and Menlo Park, California.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,774

Guelph General's COVID outbreak ends
The outbreak was declared on July 30GuelphToday Staff2 days ago

Listen to this article
00:00:42
After two weeks, the COVID-19 outbreak at Guelph General Hospital is over as of Tuesday.
The outbreak was first declared on July 30. While it wasn’t known how many patients or staff were impacted, an outbreak is when two or more people with a common epidemiological link test positive for the virus.
During the outbreak, people were asked not to visit the hospital if they had COVID-19 symptoms, and any patient with COVID-19 was not allowed to have visitors.
The mask requirement for clinical areas was re-introduced on Aug. 1 due to the rise of COVID-19 in the community, and will remain in effect until further notice.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,775

COVID is climbing in Michigan, but this summer surge is different
Michigan hospitals are seeing more COVID cases in their emergency rooms than anytime since February.
COVID is climbing in Michigan, but this summer surge is different
- Updated: Aug. 14, 2024, 5:09 p.m.
- Published: Aug. 14, 2024, 11:37 a.m.

A stack of free COVID-19 tests delivered by the U.S. Postal Services from the federal government sits on a kitchen table in Michigan.Danielle Salisbury
Twice last week, Michigan had 2% of its emergency department and urgent care visits result in a COVID-19 diagnosis.
That might sound insignificant, but it was the first time the coronavirus was that present in local hospitals since mid-February. In fact, the state is one of 16 with at least a 10% week-over-week increase, according to CDC data.
Michigan is in the midst of a summer surge of infections, much like this time last year. However, the waves are much calmer than they were during the pandemic.
“We’re not seeing the constellation of symptoms and tragic presentation from years past,” noted Dr. Jennifer Stevenson, an emergency medicine doctor at Henry Ford Health. “Overall, COVID has mutated into a virus that’s far less dangerous than it was in the beginning.”
Michigan is reporting about 441 cases and one death from COVID per day, according to state health department data from last week.
The 3,520 cases reported the week of Aug. 3 marks the highest point since Feb. 24. Last year’s summer surge continued into late September, hitting 5,369 cases in a week before an October decline.
Because testing isn’t as official as the first years of the pandemic, case counts don’t accurately depict viral spread. Many people rely on at-home testing to determine if they’ve been infected, and don’t report their case.
That’s where the state relies on other data, like emergency room COVID diagnoses, deaths, and wastewater surveillance.
Michigan’s 2% of emergency room visitors having COVID falls just shy of the national average (2.3%). The northern Lower Peninsula (4%) and Metro Detroit (3%) regions are highest in the state.
At the Dearborn hospital where Stevenson works, she’s primarily seeing people hospitalized with COVID who have other conditions like congestive heart failure or atrial fibrillation.
Symptoms vary widely. Some people experience cold-like symptoms like a cough and congestion, while others experience gastrointestinal symptoms. Stevenson said she’s not seeing as many fever reports from COVID as in the past.
Heading into August, COVID deaths were down considerably compared to the same time last year. There were 15 reported the week ending July 27, and 13 the week ending Aug. 3.
For those who test positive, Stevenson said the recommendation is more common sense and to be considerate, rather than a steadfast rule. Avoid others when you feel sick. Be mindful of your interactions with vulnerable populations. Wear a mask if you have to be around others while you’re feeling sick.
The CDC still suggests returning to normal activities after symptoms are improving overall, and after being without fever for at least 24 hours without the use of medication.
Stevenson said five days remains a useful period to avoid others, especially if you’re symptomatic. It’s not necessary to continue testing for a negative result after that time before returning to normal activities.
“What’s going to guide us is symptoms and how we’re feeling,” she said. “You’re likely not the risk (to others) then if your symptoms have resolved.”
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,776

Covid-19 update: 1666 new cases, 26 further deaths
The number of new cases continues to drop, but there have been more deaths than last week.
Covid-19 update: 1666 new cases, 26 further deaths
4:51 pm on 12 August 2024Share this
- Share on Twitter
- Share on Facebook
- Share via email
- Share on Reddit
- Share on Linked In

Photo: 123rf.com / Composite Image - RNZ
There were 1666 new cases of Covid-19 reported in New Zealand over the week to Sunday, and 26 further deaths attributed to the virus.
Of the new cases, 1008 were reinfections.
There were 93 cases in hospital, none of whom were in intensive care.
The highest number of new cases were in Canterbury, followed by Waitemata.
The case numbers were 337 fewer than last week, when Te Whatu Ora reported 2003 new cases and 15 further deaths were attributed to the virus.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,777
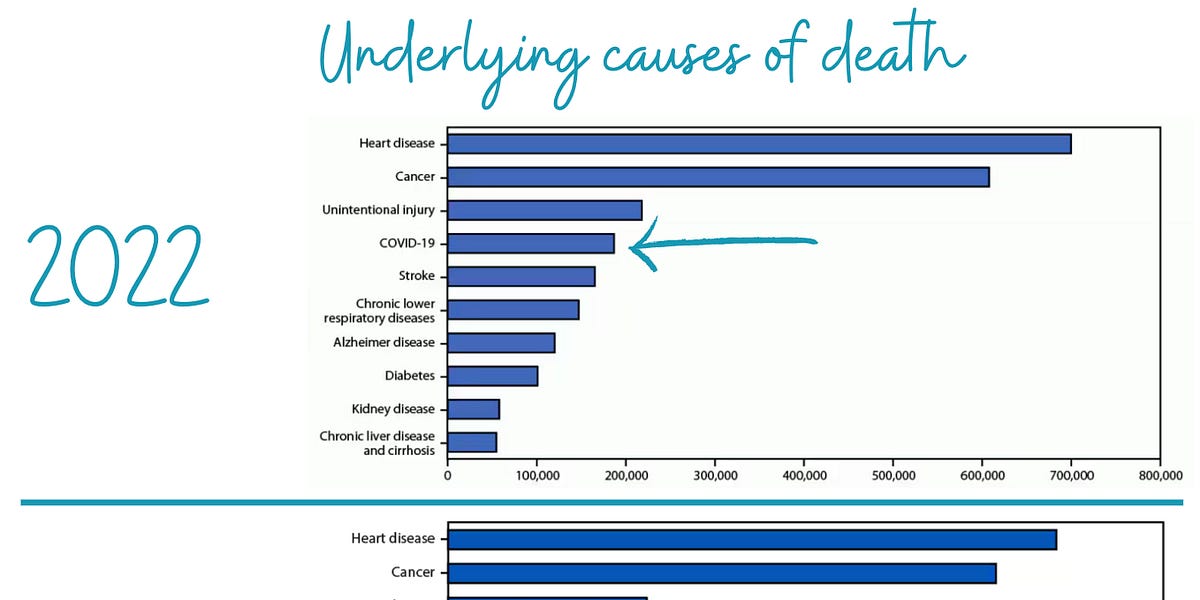
Covid-19 is now the 10th leading cause of death
And, yes, it’s still more severe than the flu.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,778

Why the Summer Olympic Games in Paris may have been a COVID 'success' story
At least 40 athletes tested positive for COVID at the Summer Olympic Games in Paris, according to the WHO. Experts say the Games are actually a COVID "success" story.
Why the Summer Olympic Games in Paris may have been a COVID 'success' story
At least 40 athletes tested positive for COVID, according to the WHO.By Mary Kekatos
August 15, 2024, 6:16 AM

Athletes who tested positive had to follow certain protocols in order to compete.
As the 2024 Summer Olympic Games in Paris came to an end this weekend, most of the conversation surrounded the number of medals won, and the number of records broken.
However, there was also another topic at hand: the presence of COVID-19 at the Olympics.
At least 40 athletes tested positive for COVID, according to the World Health Organization (WHO), including several Australian swimmers, a British swimmer and a German decathlon competitor.
Additionally, American track and field star Noah Lyles won bronze in the 200-meter race after testing positive for COVID-19 two days prior.
Despite the number of cases, public health experts told ABC News that the Paris Games were actually a success and a testament to how far the world has come since the early days of the COVID-19 pandemic in 2020.
"COVID-19 was so less disruptive in Paris than it was in Tokyo or Beijing because of what science and medicine have done over the past four years," Dr. Amesh Adalja, an infectious disease physician and senior scholar at Johns Hopkins Center for Health Security, told ABC News.
"That should be the story, that we went from something that was disrupting the entire world to something that is now kind of a rank-and-file respiratory virus. I think that's the real story. Here is the success of humanity with tackling this scientific problem, and the minds that went to work on this problem and made it something that is no longer a major concern for a lot of the population."

COVID-stricken Noah Lyles lies on the track after competing in the men's 200-meter final...Show more
Petr David Josek/AP
How the Paris Olympics were different
The Paris Olympics were billed as the first games with some sense of normalcy after the strict restrictions seen during the 2021 Summer Games in Tokyo and the 2022 Winter Games in Beijing.Athletes were under strict testing and quarantine protocols and had to follow stringent mitigation measures to participate in the 2021 or 2022 Games. No spectators were allowed at the Tokyo Games while a limited number were allowed at the Beijing Games.
Comparatively, there were no formal requirements for regular COVID-19 testing or reporting for the Paris Games, either in general or for specific events.
An athlete testing positive did not require them to sit out from an event either. Participating following a positive test was left up to the discretion of the athlete, team and medical staff. Additionally, there were no restrictions regarding spectators.
"The Paris Olympics were something that really resembled pre-COVID Olympics, nothing like what we saw in Beijing, nothing like what we saw in Tokyo," Adalja said. "And I think that reflects the fact that the context regarding the virus that causes COVID-19 has changed a lot over the past four years."
COVID at the Paris Games
Only about 40 COVID-19 cases were confirmed among athletes at the 2024 Summer Games. Experts say it's not out of the ordinary that cases would occur and that, likely, the total is an undercount of cases."I am sure that that is a gross under-representation of the actual number of cases," Dr. Pedro Piedra, a professor in the Department of Molecular Virology and Microbiology and Pediatrics at Baylor College of Medicine, Houston, told ABC News.
"[COVID] testing is not required, and testing for other respiratory viruses has really not been required either, and whenever you have such an event, it is an excellent ground for viruses to transmit. And that's not just unique to the Olympics. That's anytime you have a lot of individuals cluster over time together," he continued.
The Australian Olympic Committee said last week that 16 athletes tested positive for COVID, at least seven of whom were swimmers.

In this July 27, 2021 file photo, Simone Biles of Team United States is embraced by coac...Show more
Ezra Shaw/Getty Images, FILE
The British Olympic Committee said swimmer Adam Peaty tested positive for COVID-19 less than 24 hours after winning silver in the men's 100-meter breaststroke final.
Perhaps, most famous, Lyles -- the American sprinter -- revealed after winning bronze in the 200-meter men's final that he had tested positive two days beforehand. Lyles drew a great deal of criticism for running the race unmasked and not publicly revealing his diagnosis before the competition.
However, experts said that COVID-19 is beginning to be considered an endemic virus, meaning it is typically present, and should be treated like other endemic viruses, like the flu.
"A lot has changed, and this virus is now what we would call an endemic virus; it's basically part of the new respiratory viruses that circulate within our community," Piedra said. "We don't try to test every virus for every illness that we have. If we did, I think it would cost significantly, and on many occasions, we don't have any form of treatment or prevention methods."
Adalja said because COVID-19 is being considered an endemic respiratory virus, each individual case is less significantly important.
"We have so many tools that science and medicine have given us that make COVID-19 so much more manageable in 2024 than it was in 2020, 2021, 2022," he said. "So, in that sense, the fact that you're not hearing about every case as it occurs is just like you don't hear about every case of influenza that occurs."
He continued, "I think that the fact that people are back to their lives, that people are winning medals when they have COVID-19 really shows that despite all of the obstacles the governments put in place to deal with COVID appropriately, scientists, physicians delivered and developed so many tools that were able to now live our lives in the midst of COVID-19 and not have It be as disruptive as it once was."
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,779

In COVID-19 patients, neurological symptoms last up to three years
Scientists from Northwestern Medicine and the School of Medicine at CES University and CES Clinic in Colombia have determined that more than 60% of people who contracted COVID-19 have neurological symptoms that impact their cognitive function and quality of life, even two and three years after...
In COVID-19 patients, neurological symptoms last up to three years
Effects include brain fog, fatigue and depressionAugust 15, 2024 | By Marla Paul

Among the most significant findings, the symptoms of ‘brain fog,’ characterized by cognitive dysfunction, was experienced by 60% of patients and fatigue was experienced by 74%.
Scientists from Northwestern Medicine and the School of Medicine at CES University and CES Clinic in Colombia have determined that more than 60% of people who contracted COVID-19 have neurological symptoms that impact their cognitive function and quality of life, even two and three years after COVID-19.
This finding resulted from a study with the longest follow-up time conducted in Latin America and was led by Dr. Igor J. Koralnik, chief of neuro-infectious diseases and global neurology at Northwestern University Feinberg School of Medicine, and Dr. Carolina Hurtado Montoya, with the School of Medicine at CES University in Medellín.
This study, the first in Colombia and Latin America to analyze persistent neurological symptoms, cognitive function and quality of life in long COVID-19 patients, demonstrates that the neurologic manifestations of long COVID are as frequent in Colombia as they are in the U.S.
The process
Between April 2023 and December 2023, researchers evaluated the long-term effects of COVID-19 in a group of 100 Colombian patients, which included a group of 50 people, average age of 51, who presented moderate or severe disease and were hospitalized at the CES Clinic in Medellín. The other group of 50 patients were not hospitalized, had mild COVID-19 and were an average age of 36.Among the most significant findings, the symptoms of ‘brain fog,’ characterized by cognitive dysfunction, was experienced by 60% of patients and fatigue was experienced by 74%. These two symptoms, along with depression, most affected their quality of life and cognitive function, in both the group of patients who required hospitalization (moderate and severe COVID-19) during the acute infection, and in people who had mild COVID-19.
These results were published August 13 in Frontiers in Human Neuroscience. The research group is finalizing details to begin a second phase of the study, focused on cognitive rehabilitation, to improve the functionality and quality of life of these patients. From this new effort, researchers expect to adapt and test a protocol that can later be implemented as a service at the IPS Universidad CES in Sabaneta, Antioquia, Colombia.
The numbers
The most common neurological symptoms in patients with long COVID-19 were ‘brain fog’ in 60% of patients, muscle pain in 42% and numbness or tingling in 41%. Non-neurological symptoms were fatigue (74%), sleep problems (46%) and anxiety (44%).Both patient groups also performed worse on processing speed and attention than the general population, the study reports.
“‘Brain fog’ and fatigue remained persistent regardless of the duration of long COVID, underscoring the need for comprehensive and long-term care for those affected by this condition,” the authors wrote.
Notes
This analysis also involved medical students, physicians, neurology residents, neurologists, and researchers from CES University and CES Clinic, Diego Fernando Rojas-Gualdrón, Esteban Villegas Arbeláez, Salvador Ernesto Medina Mantilla, Mariana Campuzano-Sierra, Santiago Ospina-Patiño, Mariana Arroyave-Bustamante, Valeria Uribe-Vizcarra, Daniel Restrepo-Arbeláez, Paul Cardona, Julián Llano-Piedrahita, Santiago Vásquez-Builes, Esteban Agudelo-Quintero, Juliana Vélez-Arroyave, Sebastián Menges, as well as the team from Northwestern University including Gina S. Pérez Giraldo, Millenia Jiménez, Janet Miller and Yina M. Quique.This collaboration was initiated by Dr. Gina Perez Giraldo who went to Medical School at CES University in Medellin, and was the recipient of a Global Neurology fellowship from the Havey Institute of Global Health at Northwestern.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,780
AI reveals mental health impact of COVID-19 vaccine rollout | TechTarget
Learn how a deep learning analysis of CDC data revealed disparities in anxiety and depression prevalence among adults during COVID-19 vaccine rollouts.
AI reveals mental health impact of COVID-19 vaccine rollout
A population-based deep learning analysis of CDC data shows disparities in anxiety and depression prevalence among adults during COVID-19 vaccine rollouts.

By
- Shania Kennedy, Assistant Editor
COVID-19 vaccine rollouts disparately impacted mental health outcomes for U.S. adults according to recent research led by the University of Alabama at Birmingham (UAB) and published in The Lancet Regional Health -- Americas.
The researchers indicated that existing studies have demonstrated increased mental health issues in U.S. populations following COVID-19 outbreak, but that evidence around the impact of the various phases of COVID-19 vaccine rollout on mental health is lacking.
To help close this evidence gap, the research team conducted a population-based multi-intervention interrupted time series analysis via deep learning to analyze four waves of data from the CDC Behavioral Risk Factor Surveillance System.
This information, representing data points from January 2019 to February 2023, was then used to analyze changes in the prevalence of anxiety and depression in adults following each major COVID-19 vaccine rollout phase from 2020 to early 2023.
The findings revealed both positive and negative mental health impacts related to vaccine rollout, and rates of both depression and anxiety generally declined among the general population.
Significant reductions were experienced by particular subgroups during different rollout phases: women reported lower anxiety and depression across multiple phases, and individuals raising children saw mental health improvements tied to the availability of vaccines for children and childcare workers.
Similarly, adults reporting poor physical health saw improvements in depression and anxiety coinciding with the rollout of booster shots.
However, the study also highlighted mental health disparities among some marginalized groups, including Black and non-Hispanic people of color, alongside those with lower incomes. These populations saw increases in anxiety and depression during the initial vaccine rollout, likely due to factors like mistrust, discrimination and pandemic-related economic hardship.
"Concerns about the vaccine's safety and effectiveness were more pronounced in these communities, partly due to past experiences of being mistreated or misled by health care providers and authorities," explained Yusen Zhai, Ph.D., lead author and director of the UAB Community Counseling Clinic, in a news release. "This skepticism was exacerbated by the fast-paced development and distribution of the vaccine, making it harder for people to feel confident about getting vaccinated."
The research team emphasized that these findings underscore the need to prioritize both mental and physical health -- through strategies like vaccine shortage planning and provision of mental health resources -- in population health management efforts for infectious disease.
"The empirical evidence gleaned from this study suggests the disparate effects of the phased vaccine rollout on mental health across U.S. populations, underlining the need for careful planning in future strategies for phased disease prevention and interventions," Zhai said.
Yommie
Elite Member
- Oct 2, 2013
- 64,163
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #1,781

Uninsured? Experts Explain How to Get Your Free COVID Shot Before the Money Runs Out | KQED
The federal program that funds free COVID vaccines for those without health insurance is ending several months earlier than expected – and medical experts are advising uninsured people to get their shots before the money runs out for good.
Uninsured? Experts Explain How to Get Your Free COVID Shot Before the Money Runs Out
Carly Severn
Aug 15
Save Article

A registered nurse with The Los Angeles Department of Public Health administers a COVID vaccination at The Village Mental Health Services in Los Angeles in August 2022. (Christina House/Los Angeles Times via Getty Images)
The federal program that funds free COVID vaccines for people without health insurance is ending several months earlier than expected – and uninsured folks are now being told it could be their last chance to seek out a free shot before the money runs out for good.
The Bridge Access Program was launched by the Centers for Disease Control and Prevention (CDC) in September 2023, to provide free COVID vaccinations to the estimated 25-30 million adults in the U.S. without health insurance. The funds were previously forecast to last until December, and would have made COVID vaccines accessible to uninsured people through the brunt of another winter respiratory virus season.
But after March negotiations in Congress resulted in $4.3 billion being withdrawn from the Department of Health and Human Service’s COVID fund, the program is instead ending this month, months ahead of schedule.
The CDC has given no firm deadline for the end of the program beyond “August 2024,” and has yet to respond to KQED’s request for more specific details.
But in a statement, the California Department of Public Health said that the program is “scheduled to end when the new 2024-2025 COVID-19 vaccines are approved by the federal government.” According to drug manufacturers Pfizer and Moderna, these updated fall COVID vaccines, which will be targeted to the latest variants, could be ready as early as this month.
Sponsored
Finding locations that offer free COVID shots has also become more difficult for those without insurance, even though the Bridge Access Program funding is technically still in place. The CDC’s online vaccine locator tool, which previously offered people a way to search for nearby vaccination sites and filter by whether they were participating in the program, has now been removed from vaccines.gov.
A message on that site now states that the vaccine locator will be replaced with a pharmacy lookup tool that “will be added once 2024-2025 flu and COVID-19 vaccines become widely available.” But the site does not currently appear to offer any way to find free vaccination locations.
Keep reading for what to know about COVID shots for uninsured people, or jump straight to how to find a free vaccine if you don’t have health insurance.
As funding dries up, clinics are left scrambling
“We didn’t get any specific advance notice of exactly when it was going to be happening,” said Dr. Michael Stacey, chief medical officer at LifeLong Medical Care – one of the community clinics that’s been offering free COVID shots to uninsured people through the Bridge Access Program. “Our notification came along with the rest of the rest of the world.”The federal program launched when the commercial health care market began taking over COVID vaccine distribution from the federal government – which had until then made the vaccines free to everyone, regardless of insurance. This means that like the flu shot, a person’s COVID vaccine is now either paid for under their health insurance plan if they have one, or through a sizable out-of-pocket payment. At CVS, for instance, a COVID vaccine costs $190.99 if you don’t have any insurance.
The Bridge Access Program was one of the few remaining sources of pandemic-era funding to offer COVID care to “the most vulnerable in the community,” said Stacey, who noted that the timing is particularly unfortunate due to the ongoing nationwide summer surge in infections.
Uninsured children, ages 18, however, and under can still get free COVID vaccines and other free immunizations as part of the Vaccines for Children Program.
During a visit this week to the Petaluma Health Center – one of the clinics that’s still offering free COVID shots for uninsured people – U.S. Secretary of Health and Human Services Xavier Becerra, said he “believe[d] the clinics, the community health centers will continue to have shots” after the program’s funding ends. But he did not offer any specifics on how the clinics could continue to offer them.
Locations like the Petaluma Health Center say they are now seeking grants, along with county and state funding, to make sure they can keep offering free vaccines.
Should uninsured people seek a free shot ASAP before the funding runs out?
For Dr. Stacey, of Lifelong Medical Care, the answer is simple: Yes. “For those that don’t have insurance, try to get the vaccine now before the [Bridge Access] program ends,” he said.“We’re plugging ahead in these last days that we have to be able to vaccinate the uninsured as much as we can before the program actually shuts off,” Stacey said.
Dr. Peter Chin-Hong, an infectious disease expert at UCSF, echoed that, telling KQED by email that it’s “100% true that uninsured people should try to get the vaccine now, given the uncertainty of what will happen in the fall” regarding the program’s funding..
more on covid vaccines
COVID Booster Rollout Slowed by Distribution, Insurance Issues
You’re Not Imagining It: COVID Cases Are Up Again
California’s COVID Emergency Ends Feb. 28
The COVID vaccine that’s currently available has been around since September 2023 (and this spring, an extra shot of the vaccine formulation was recommended for people age 65 and older.) The new, updated COVID vaccine targeted to the latest variants is scheduled for release this fall, with Pfizer and Moderna both saying their vaccines could be ready as early as this month.
But Chin-Hong says that just because a new vaccine is expected soon, uninsured people shouldn’t be dissuaded from getting the current vaccine for free now – not just because the money for free shots is about to run out, but also because it’s not necessarily the best idea to get the new shot the minute it’s released anyway.
Even though the CDC recommends that you wait two months between COVID shots, “you won’t want to get the vaccine when it comes out immediately anyway as it is meant for the expected onslaught of cases in the winter,” Chin-Hong said. “Get it too soon, and your maximal antibodies will peak before you need it.”
And amid current high infection rates, there’s data to indicate that the available COVID vaccine still offers good protection against the latest variants causing this surge, even though it was originally targeted to older variants, Chin-Hong said.
“The superpower of the vaccine is to protect against serious disease, hospitalization and death,” he said. “And for that, even the [current] XBB.1.5 booster will perform spectacularly well.”
Getting the current COVID vaccine now for free might also buy uninsured folks some time – and extra immunity – as public health agencies work out how to continue extending access to them, said Chin-Hong.
“Uninsured people who get the vaccine now can rest assured that the vaccine will likely protect against serious disease for at least a year,” he said. “So even if there are problems with getting the new vaccine in the fall, I feel comfortable that many of those can take this immune system reminder to carry them through the winter reasonably well.”
How can I find a free COVID shot ASAP if I’m uninsured?
Like many aspects of finding COVID care at this stage of the pandemic, even finding a location that offers free COVID vaccines to uninsured people through the Bridge Access Program has become more difficult – especially since the CDC removed its online vaccine locator tool that showed all Bridge Access Program sites from vaccines.gov.So if you’re uninsured and want to find a free COVID shot as soon as possible before the program funding runs out, here’s a selection of options. Unfortunately, a number of them now require proactive research and action.
Use the state’s My Turn Vaccine Locator
This online tool from the California Department of Public Health allows you to filter by vaccine type and insurance status. However, this tool does not show every single vaccination site that may offer free shots through the Bridge Access Program for those without insurance. For example, it only returns two clinics that offer COVID shots to uninsured people within 50 miles of San Francisco (in Napa and San Jose).
Find a community health center through the U.S. Department of Health and Human Services (HHS)
HHS has a map tool showing community health centers that may offer free COVID shots for uninsured people. After you search for a nearby location, contact that center directly to ask if its offering no-insurance COVID shots for free through the Bridge Access Program.
The San Francisco Department of Public Health (SFDPH) also says that its AITC Immunization and Travel Clinic provides the COVID vaccine to uninsured people, although the agency notes that “people outside of San Francisco are encouraged to contact their local health department to find a vaccine near them.” The clinic is located at 101 Grove Street, Room 102, and appointments are required: call 415-554-2625 for hours and availability.
SFDPH also recommends that uninsured people visit the appointment-only San Francisco Free Clinic (4900 California Street; call 415-750-9894 for hours and availability). But when you call, check if you need to be a SF resident to receive a free COVID vaccine.
Reach out to your local pharmacy
Both the California Department of Public Health and SFDPH recommend you directly contact pharmacies near you to ask if they have COVID vaccines in stock and whether they’re offering those shots for free through the Bridge Access Program.
Remember to be really careful and confirm, repeatedly, that any shot will actually be free, as the out-of-pocket cost can be steep.
Reach out to your local health department
Contact your city or county’s public health department to ask if they’re still offering free COVID vaccines to folks without insurance through the Bridge Access Program or otherwise. The following links may also provide information on community clinics offering vaccines – just be sure to stress you don’t have insurance and are looking for free shots.
- Alameda County COVID vaccination
- City of Berkeley COVID vaccination
- Contra Costa COVID vaccination
- Marin County COVID vaccination
- Napa County COVID vaccination
- San Francisco COVID vaccination
- San Mateo County COVID vaccination
- Santa Clara County COVID vaccination
- Solano County COVID vaccination
- Sonoma County COVID vaccination
What’s going to happen with free COVID vaccinations for uninsured people in the long run?
It’s still unclear.In a recent statement, the California Department of Public Health says they are “exploring options to continue to support COVID-19 vaccine access after the end of the BAP program for uninsured and underinsured adults, including limited federal and state funding sources,” and that vaccine manufacturers “may also develop patient assistance programs.”
The agency, is said, “remains committed to monitoring vaccine access options for vulnerable populations including uninsured adults and will share relevant information as it becomes available.”
Dr. Stacey, of Lifelong Medical Care, says that in the absence of official guidance, clinics like his are “going to work on seeing what we can do to get funding and get resources to be able to continue, hopefully in the near future, to be able to provide the vaccines to the uninsured again.”
“We are trying to figure out how we can get funding or be able to purchase at least a limited supply of vaccines that we can use for those who are experiencing homelessness,” he said. “We don’t have a solution to that right now. Not only are the vaccines not being provided to us through this program, but the cost of the vaccines has also gone up.”
Dr. Chin-Hong, of UCSF, is optimistic that in the fall, Bay Area and statewide public health officials “will likely find a way to get the new COVID vaccine into uninsured arms,” since he’s found those agencies “generally more forward thinking” and willing to “provide more safety net programs than many other areas in the country.”
“However,” he cautions, “it will take some time for these programs to roll out smoothly.”
Users who are viewing this thread
Total: 1 (members: 0, guests: 1)
Pakistan Defence Latest
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (3 Viewers)
- Latest: SteppeWolff
-
-
-
