Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,012

Summer travel is fueling California's COVID surge. Labor Day will be big test
The rate at which coronavirus tests are coming back positive continues to rise in California.
Summer travel is fueling California’s COVID surge. Labor Day will be big test

Travelers make their way through Tom Bradley International Terminal at LAX in July.
(Jason Armond / Los Angeles Times)
By Rong-Gong Lin II
and Seema Mehta
Aug. 27, 2024 8:33 AM PT
CHICAGO —
Summer travel is helping fuel a COVID surge across California and other parts of the country.
There are growing reports of attendees at the Democratic National Convention getting COVID-19. At least a dozen people from California — delegates, political strategists and news reporters — said they tested positive after the DNC ended last week in Chicago.
Democratic strategist Tracy Austin, who caught COVID while attending the convention, told The Times: “It was an amazing time, but the DNCC last week stood for the Democratic National COVID Convention.”
ADVERTISING
The next big test for the COVID spike is just around the corner.
Doctors will be closely watching to see whether the back-to-school season and the Labor Day holiday weekend worsen the surge. Last week, officials with the U.S. Centers for Disease Control and Prevention said some data suggest a slowing of new coronavirus infections in some parts of the country. But a dip in the summer surge won’t be obvious until there are several weeks of sustained declines — which hasn’t happened yet.

California
As COVID wave wallops California, new vaccines arrive this week. Will it be a turning point?
Aug. 26, 2024Packed airports and large indoor events have long been shown to increase the spread of the coronavirus, and this summer has broken travel records. The Transportation Security Administration said June 23 resulted in the most passengers screened on a single day since the agency’s creation: 2.99 million. Southern California airports also have reported big increases in passenger volume.
Many DNC events occurred indoors, where the infection risk for large groups is greatest.
“That’s going to happen any time nearly 25,000 people are packed into an arena, in hotels and on shuttle buses for four days, no matter what the occasion is,” said California Democratic Party spokesperson Robin Swanson. “But the biggest takeaway from our convention is enthusiasm to elect Democrats across the country.”
Advertisement
Dr. Elizabeth Hudson, regional chief of infectious diseases at Kaiser Permanente Southern California, said her first thought as a physician in watching the DNC was, “Oh, no, hardly anyone is wearing a mask.”
She said she remembered thinking, “There’s probably going to be an awful lot of cases of COVID that come from this.
“You get a lot of people together in an indoor area who are talking and laughing and shouting, which is actually a more efficient way to spread COVID,” Hudson said. “Between all of that ... exposure time, definitely, we are certainly going to see COVID.”
Advertisement
Even though masks have gone out of fashion, they remain an effective tool in helping to prevent COVID-19, along with avoiding sick people, spending more time outdoors or in well-ventilated areas, washing or sanitizing your hands frequently and staying up to date on vaccinations.
“When you are traveling, if you’re going to be in an indoor area with an awful lot of people, to really reduce your your risk of becoming COVID-positive, you really should be wearing a mask,” Hudson said.
And “if you’re on a plane, if you’re in an airport, those are the times you really want to make sure that you are wearing a mask,” she added.
Science & Medicine
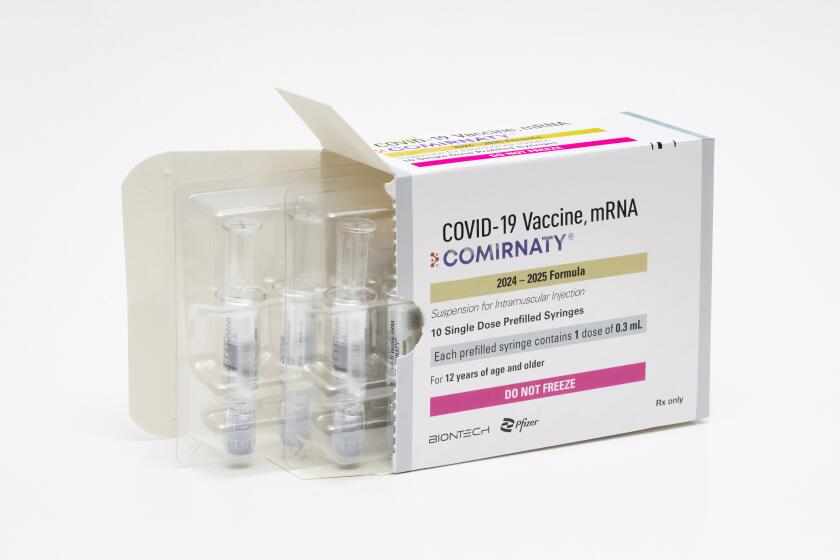
FDA approves updated COVID-19 vaccines; shots should be available in days
Aug. 22, 2024The updated COVID-19 vaccinations for the 2024–25 season are expected to become available as soon as this week, and everywhere sometime in September.
There are a number of reasons why this summer COVID wave has been surprisingly strong.
One is the emergence of successive hyperinfectious coronavirus subvariants. In the spring, some of the subvariants collectively nicknamed FLiRT, including KP.2, began a midyear wave. That was followed by ever-more-contagious successor subvariants — KP.3 (nicknamed FLuQE, pronounced “fluke”) — and the latest, KP.3.1.1 (nicknamed deFLuQE, pronounced “de-fluke”).
In the latest subvariant, KP.3.1.1, “the particular variation that came up in this mutation was a little different than what people had either seen with either natural immunity or with the vaccinations that we had available,” Hudson said.
“Because of that, it just made it much more easy to come into a population where people’s natural and vaccine-induced immunity was at a nadir,” Hudson said, with many people nearly a year or more out from their last immunization or their last COVID-19 illness.
There are now 26 states, including California, where COVID-19 is projected to be “growing” or “likely growing.” That’s down from 44 states about six weeks ago, according to the CDC.
The rate at which coronavirus tests are coming back positive continues to rise in California. For the week that ended Aug. 19, 14.4% of reported tests were positive. That’s higher than the peaks seen last summer and winter, and up from about 11.5% a month ago.
Overall, coronavirus levels in California’s wastewater have been largely flat in recent weeks, but remain at the season’s highest level.
COVID levels in California sewage may be starting to plateau
Weekly wastewater viral activity levelLine chart shows COVID levels in wastewater. For the week ending on Aug. 17, the California level is 12.43, considered very high. Nationwide, the level is very high at 8.68.
California
U.S.
Viral activity level categoriesVery high High ModerateLow MinimalLatest data is for the week ending on Aug. 17.
U.S. Centers for Disease Control and Prevention
Sean Greene
Los Angeles Times
How to protect yourself
- Test if you’re sick — and test daily. It’s sometimes taking longer after the onset of illness for a rapid test to show positive. If an initial test is negative, you may still have COVID. Consider retaking tests daily, up to five days after the onset of cough-and-cold symptoms, Hudson said. A positive test can help you take measures to isolate quicker and limit spread of the illness.
- Have a plan to ask for Paxlovid if you become ill. Paxlovid is an antiviral drug that, when taken by people at risk for severe COVID-19 who have mild to moderate symptoms, reduces the risk of hospitalization and death. There are also other anti-COVID drugs, such as molnupiravir, which is also taken orally, and remdesivir, which is administered intravenously.
- People who are moderately or severely immunocompromised can also get a medicine called pemivibart, whose brand name is Pemgarda. Given intravenously in a medical facility over an hour, the drug helps prevent COVID-19 before someone is exposed to the virus, but doesn’t replace vaccines.
- Wearing a mask, particularly on a crowded flight or other indoor venues, can help reduce the risk of infection.
- The CDC says people should stay away from others until at least 24 hours after their symptoms are getting better and they have not had a fever (and are not using fever-reducing medicine). The agency suggests taking added precautions for five days — like wearing a well-fitting mask and continuing to test for COVID, in case of viral rebound — to avoid sickening other people.
- Besides the CDC guidance, the Los Angeles County Department of Public Health also recommends testing yourself using a rapid test, and getting a negative result, before leaving isolation. The agency recommends masking for 10 days around other people after you start feeling sick, or if asymptomatic, your first positive COVID test. You can unmask earlier if you have two sequential negative COVID tests, taken at least a day apart. The agency also suggests staying away from the elderly and immunocompromised people for 10 days after you start to feel sick.
- Generally, tips like these also reduce the risk of a coronavirus infection: keeping distance from other people, increasing air circulation by opening windows, turning on air purifiers, gathering outdoors if meeting with people, and sticking with enhanced hygiene: washing and sanitizing hands often, cleaning high-touch surfaces, and covering coughs and sneezes.

California
‘A much more infectious’ COVID variant fueling California’s relentless surge
Aug. 19, 2024
Additional travel tips from the CDC
- Make sure you are up to date on all of your routine vaccines; they protect from infectious diseases, such as measles, that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.
- Get up to date with your COVID-19 vaccines and get a seasonal flu vaccine. In the U.S., the CDC recommends getting COVID and flu vaccines in September or October.
- Prepare a travel health kit with items you may need, especially those that may be difficult to find at your destination. Include prescriptions and over-the-counter medicines and take enough to last your entire trip, plus extra in case of travel delays. Depending on your destination, you may also want to pack a mask, insect repellent, sunscreen (SPF 15 or higher), aloe, alcohol-based hand sanitizer, water disinfection tablets and your health insurance card.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,013

Canadian Public Health has Spoken
Apparently we’re all in with Pfizer and Moderna despite Novavax providing significantly better protection and fewer risks.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,014
FDA approves the latest COVID booster shots but there is no push for mass vaccination
The FDA approved the latest COVID vaccine boosters on the tail end of the Democratic National Convention that can best be characterized as a superspreader event. Meanwhile, more than 1.3 million people are being infected daily with COVID.
www.wsws.org
FDA approves the latest COVID booster shots but there is no push for mass vaccination
Benjamin Mateus
The US Food and Drug Administration (FDA) approved and granted emergency use authorization Thursday for updated mRNA COVID-19 vaccines developed by Pfizer, Moderna and Novavax. The action came on the final day of the Democratic National Convention in Chicago, one of innumerable superspreader events being held with the full support of the Biden-Harris administration and public health officials, who have abandoned any serious effort against the pandemic.The DNC nominated Vice President Kamala Harris as its presidential candidate, after a four-day celebration in which the COVID pandemic was portrayed as something in the rear-view mirror, an accomplishment for President Biden to boast about when it was even mentioned (rarely).
The truth is, however, that Biden is already responsible for far more COVID deaths than his predecessor. At a 2020 debate, Biden correctly said that the 200,000 deaths of Americans that had already occurred should disqualify President Trump from remaining in the White House. By the time Biden departs the White House next January, the death toll during his four-year term could well be more than one million people.
The last thing any Democratic Party politician wanted to do was to stand before the convention and a national television audience and talk about the daily toll from the pandemic, now estimated to be 1.3 million new cases per day, with nearly 100 deaths. And this before the return of students to the classrooms and college campuses.
According to modeling estimates by Dr. Mike Hoerger on national SARS-CoV-2 wastewater concentrations, there have been 179 million COVID infections in the US just in 2024. He noted, “Keep in mind, November and December will be particularly bad, and now through October is still bad too.” By comparison, in all of 2023, 248 million Americans were infected, or roughly three-quarters of the population. At the current rate, 2024 could surpass that. In all, he estimated that there have been more than 1.1 billion infections, just in the United States, since the start of the pandemic.
Meanwhile, emergency room visits, hospitalizations and deaths have been climbing since the lows in May 2024. Deaths are up to 690 per week as of the end of July, up nearly 20 percent from the same point the previous year. Presently, 26,000 people have died from COVID in 2024 thus far. At this rate between 50,000 and 60,000 deaths acute deaths can be expected not accounting for excess deaths or those caused by health complications as result of infection or reinfection.
Why weren’t public health efforts advanced when the summer surge indicated not everything was well? Why weren’t the vaccines made available then?
Simply put, the Centers for Disease Control and Prevention (CDC) and the FDA were told not to rock the boat which the Biden administration devoted its efforts to promoting war and nationalism, ending the social spending triggered by the COVID emergency and funneling these funds into military aid to Ukraine, support for Israel in Gaza, and a further build-up against China in the Indo-Pacific.
Although the FDA had advised manufacturers in June that they should use the JN.1 strain for their latest formulation, rapid viral evolution spawned the KP.2, KP.3, and KP.3.1 strains that are now dominant in the US, compelling the agency to request Pfizer and Moderna to utilize the KP.2 strain, “if feasible.” Even this version of the vaccine is trying to catch the tail of a fast-moving target. The KP.2 variant of SARS-CoV-2 now accounts for less than three percent of all currently sequenced viral genomes.
Even the New York Times, the semi-official publicist for the forever COVID policy, offered the following accurate assessment of the state of the ongoing pandemic:
In the FDA statement informing of the EUA approval, Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, wrote:For the frailest Americans, who have been dying of COVID in growing numbers this summer, the shots could offer a reprieve from a virus that disproportionately endangers those whose vaccinations are out of date. But the approval is occurring months after wily new variants began driving up infections, a matter of consternation for some scientists who have urged faster turnabouts for updated shots.
Despite the limitations, the uptake of the vaccines is vital for the health of the population. The shots have a strong, proven safety record and do prevent severe disease and potentially reduce the risk of Long COVID, as studies have indicated. However, they do not prevent infections and the immunity they offer is short lived given the the constant mutation of the virus. Therefore, the FDA assertion that “vaccinations are a cornerstone of COVID-19 prevention” is false and foments public mistrust.Vaccination continues to be the cornerstone of COVID-19 prevention. These updated vaccines meet the agency’s rigorous, scientific standards for safety, effectiveness and manufacturing quality. Given waning immunity of the population from previous exposure to the virus and from prior vaccination, we strongly encourage those who are eligible to consider receiving an updated COVID-19 vaccine to provide better protection against currently circulating variants.
The only real preventive measure is a systematic public health mobilization to eliminate the virus. Stopping SARS-CoV-2 from continually spreading through the population remains feasible and is the only scientific solution to the growing public health crisis posed by Long COVID, which has become the most common ailment across the globe. A recent study by Long COVID expert Dr. Ziyad Al-Aly estimated that by the end of 2023, there were at least 410 million people with Long COVID. The study put the global economic cost of the condition at about $1 trillion annually.
The boosters from Pfizer and Moderna are expected to be available at pharmacies by the first week of September for those six months of age and older. Novavax, which uses the virus’s spike protein instead of the mRNA, as a target for the immune system, expects its updated version to be available later.
Children ages 5 to 11 wait in line with their parents to receive the Pfizer COVID-19 vaccine at a pediatric vaccine clinic set up at Willard Intermediate School in Santa Ana, Calif., Nov. 9, 2021. [AP Photo/Jae C. Hong]
Mehring Books
COVID, Capitalism, and Class War: A Social and Political Chronology of the Pandemic
A compilation of the World Socialist Web Site's coverage of this global crisis, available in epub and print formats.
Buy your copy today
However, with the Federal Bridge Access Program set to end on August 31, 2024, the 26 million uninsured and tens of million more with inadequate coverage, an estimated 43 percent of adults age 19 to 64, will have to weigh the decision to obtain a vaccine that costs between $120 to $130 per dose. A Kaiser Family Foundation analysis from February 2024, estimated that people in the US owe at least $220 billion in medical debt;14 million owe over $1,000 and about three million owe more than $10,000.
Given the abysmal rates of vaccination last year, the end of the program will only mean that the current campaign to get people vaccinated will have little success. The year-to-year trend is unmistakeable.
On October 22, 2022, six weeks after the first bivalent COVID boosters were introduced, more than 18 million people received the vaccines. By mid-October 2023, six weeks after the second iteration of the COVID boosters was introduced, only seven million Americans had taken the vaccines. By the four-month mark, or mid-January 2024, at the height of the winter wave, only 20 percent of the population had received a booster.
As a Minneapolis physician, Dr. Zeke McKinney recently observed, “We don’t have the community push or diffusion of vaccines the way we once did. It’s mostly up to everyone on their own to figure it out.”
In its report on the FDA approval and the roll-out of the COVID boosters, the Times wrote, the prospects of any meaningful impact “remains dim... The availability of boosters has not translated into actual vaccinations. By spring, only one in five adults had received last year’s updated Covid vaccine. Even older Americans, who are at far greater risk of being severely sickened, largely spurned the shots, with only 40 percent of people 75 and older taking last year’s vaccine.”
Nursing homes and long-term care facilities have seen a significant delay and decline in their vaccination status. According to the CDC’s dashboard, as of the end of July, only 31 percent of nursing home residents are up to date on their COVID-19 vaccines.
Contrary to the suggestion of the Times, the blame for the poor uptake of vaccine boosters cannot be placed on the elderly, and still less on nursing home residents. The main reason is the lack of resources to make vaccines available, and the desire of the corporate elite to look on the “bright side” of the pandemic.
Mass death among the elderly, the infirm, and the immuno-compromised is viewed as a positive good by the financial aristocracy, which begrudges every penny spent to keep people alive who no longer produce profits for the capitalist class. This homicidal logic is increasingly embraced by the capitalist politicians of both parties.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,015
On the Covid ‘Off-Ramp’: No Tests, Isolation or Masks
For many, Covid is increasingly regarded like the common cold. A scratchy throat and canceled plans bring a bewildering new critique from friends: You shouldn’t have tested.
By Emily Baumgaertner
Emily Baumgaertner, the national health correspondent, has a graduate degree in public health and has covered Covid since 2020.
Aug. 27, 2024 Updated 11:48 a.m. ET
Jason Moyer was days away from a family road trip to visit his parents when his 10-year-old son woke up with a fever and cough.
Covid?
The prospect threatened to upend the family’s plans.
“Six months ago, we would have tested for Covid,” Mr. Moyer, 41, of Ohio, said. This time they did not.
Instead, they checked to make sure the boy’s cough was improving and his fever was gone — and then set off for New Jersey, not bothering to tell the grandparents about the incident.
In the fifth summer of Covid, cases are surging, and the Centers for Disease Control and Prevention has reported “high” or “very high” levels of the virus in wastewater in almost every state. The rate of hospitalizations with Covid is nearly twice what it was at this time last summer, and deaths — despite being down almost 75 percent from what they were at the worst of the pandemic — are still double what they were this spring.
As children return to schools and Labor Day weekend travel swells, the potential for further spread abounds. But for many like Mr. Moyer, Covid has become so normalized that they no longer see it as a reason to disrupt social, work or travel routines. Test kit sales have plummeted. Isolation after an exposure is increasingly rare. Masks — once a ubiquitous symbol of a Covid surge — are sparse, even in crowded airports, train stations and subways.
Human behavior is, of course, the reason that infections are soaring. But at some point, many reason, we need to live.
“I no longer even know what the rules and recommendations are,” said Andrew Hoffman, 68, of Mission Viejo, Calif., who came down with respiratory symptoms a few weeks ago after his wife had tested positive for Covid. He skipped synagogue, but still went to the grocery store.
“And since I don’t test, I can’t follow them,” he said.
Epidemiologists said in interviews that they do not endorse a lackadaisical approach, particularly for those spending time around older people and those who are immunocompromised. They still recommend staying home for a couple of days after an exposure and getting the newly authorized boosters soon to become available (despite the poor turnout during last year’s round).
But they said that some elements of this newfound laissez faire attitude were warranted. While Covid cases are high, fewer hospitalizations and deaths during the surges are signs of increasing immunity — evidence that a combination of mild infections and vaccine boosters are ushering in a new era: not a post-Covid world, but a post-crisis one.
Epidemiologists have long predicted that Covid would eventually become an endemic disease, rather than a pandemic. “If you ask six epidemiologists what ‘endemic’ means, exactly, you’ll probably get about 12 answers,” said Bill Hanage, associate director of the Center for Communicable Disease Dynamics at Harvard T. H. Chan School of Public Health. “But it certainly has a sort of social definition — a virus that’s around us all the time — and if you want to take that one, then we’re definitely there.”
Certain threats remain clear. For vulnerable groups, the coronavirus will always present a heightened risk of serious infection and even death. Long Covid, a multifaceted syndrome, has afflicted at least 400 million people worldwide, researchers recently estimated, and most of those who have suffered from it have said they still have not recovered.
But the C.D.C. director, Dr. Mandy Cohen, called the disease endemic last week, and the agency decided earlier this year to retire its five-day Covid isolation guidelines and instead include Covid in its guidance for other respiratory infections, instructing people with symptoms of Covid, RSV or the flu to stay home for 24 hours after their fever lifts. The updated guidelines were an indicator that, for most people, the landscape had changed.
Dr. Hanage defended the hard-line mandates from the early years of the pandemic as “not just appropriate, but absolutely necessary.”
“But,” he said, “it is just as important to help people onto an off-ramp — to be clear when we are no longer tied to the train tracks, staring at the headlights barreling down.”
The absence of stringent guidelines has left people to manage their own risks.
“I don’t bother testing myself or our kids for Covid,” said Sarah Bernath, 46, a librarian on Prince Edward Island in Canada. “My husband doesn’t test himself either. Knowing if it’s Covid wouldn’t change whether I stay home or not.”
In some social circles, diverging choices can make for uncomfortable dynamics.
Debra Cornelius, 73, of Carlisle, Pa., stayed home from a recent indoor party because she learned that several other guests — a family of five — had returned from vacation and tested positive for Covid three days before the gathering, but still planned to attend.
“They said, ‘Oh, it’s like a bad cold, we wouldn’t stay home for a cold,’” she said. “I think people’s attitudes have changed considerably.”
Four years ago, social distancing stickers on floors of hotels, banks and other public places were widely used.
But for countless others, attitudes haven’t changed at all. Diane Deacon, 71, of Saginaw, Michigan, said she tested positive for Covid three days into a trip to Portugal with her two adult daughters. She isolated herself for five days before flying home wearing a mask.
“A number of people asked me, ‘Why did you test? You could have carried on with your vacation,’” she said.
For Ms. Deacon, it was about remembering the refrigerated morgue trucks of 2020 and anticipating the vulnerable people she might see on her flight home — people in wheelchairs, or people on oxygen, she said.
“I’m trying to avoid a moral judgment of people who make other choices,” she said. “To me, it was inconvenient and it was unfortunate, but it was not a tragedy.”
In a Gallup poll this spring, about 59 percent of respondents said they believed the pandemic was “over” in the United States, and the proportion of people who said they felt concerned about catching Covid has been generally declining for two years. Among people who rated their own health positively, almost 9 in 10 said they were not worried about getting infected.
That could be, at least partly, a result of personal experience: About 70 percent of people said they had been through a Covid infection already, suggesting that they believed they had some immunity or at least that they could muscle through it again if need be.
If the Olympics were any barometer, the rest of the world seems to have exhaled as well. In Tokyo in 2021, there were daily saliva samples, plexiglass dividers between cafeteria seats and absolutely no live spectators; the arenas were so empty that coaches’ voices echoed. In Beijing in 2022, under China’s zero-tolerance policy, conditions were much the same.
But in Paris last month, the organizing committee for the 2024 Olympics offered no testing requirements or processes for reporting infections, and so few countries issued rules to their athletes that the ones that did made news.
There were high-fives, group hugs, throngs of crowds and plenty of transmission to show for it. At least 40 athletes tested positive for the virus, including several who earned medals in spite of it — as well as an unknowable number of spectators, since French health officials (who had once enforced an eight-month-long nightly Covid curfew) did not even count.
The closing ceremony of the Olympic Games in Paris, where more than 40 athletes reported Covid infections and some, like Noah Lyles, competed while sick.
New York’s straphangers have returned to the subways, in contrast to the lockdown days, when trains often ran with entirely empty cars.
In the United States, about 57 percent of people said their lives had not returned to prepandemic “normal” — and the majority said they believed it never would. But the current backdrop of American life tells a different story.
The years-old social-distancing signage is faded and peeling from the floors of an indoor market in Los Angeles. Hand-sanitizer dispensers at amusement parks have dried up. The summer camp hosted by Chicago’s Lincoln Park Zoo requires children to bring a face covering — not to protect other children, but the animals.
Michael Osterholm, the director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said the newfound complacency can as much be attributed to confusion as to fatigue. The virus remains remarkably unpredictable: Covid variants are still evolving much faster than influenza variants, and officials who want to “pigeonhole” Covid into having a well-defined seasonality will be unnerved to discover that the 10 surges in the United States so far have been evenly distributed throughout all four seasons, he said.
Those factors, combined with waning immunity, point to a virus that still evades our collective understanding — in the context of a collective psychology that is ready to move on. Even at a meeting of 200 infectious disease experts in Washington earlier this month — a number of whom were over 65 and had not been vaccinated in four to six months — hardly anybody donned a mask.
“We’ve decided, ‘Well, the risk is OK.’ But nobody has defined ‘risk,’ and nobody has defined ‘OK,’” Dr. Osterholm said. “You can’t get much more informed than this group.”
Asked about how the perception of risk has evolved over time, Dr. Osterholm laughed.
“Lewis Carroll once said something like, ‘If you don’t know where you’re going, any road will take you there,’” he said. “I feel in many ways, that’s where we’re at.”
Last edited:
Khansaheeb
Elite Member
- Dec 14, 2008
- 19,909
- 20,959
- Country of Origin

- Country of Residence

Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,021

High rates of COVID are causing outbreaks, rising hospitalizations and deaths heading into the school year
Health Canada expediting review of vaccines targeted at new COVID variants driving the surge.
High rates of COVID are causing outbreaks, rising hospitalizations and deaths heading into the school year
Health Canada expediting review of vaccines targeted at new COVID variants driving the surge.Get the latest from Elizabeth Payne straight to your inbox
Author of the article:
Elizabeth Payne
Published Aug 27, 2024 • Last updated 8 hours ago • 5 minute read
41 Comments

Article content
If it seems like many of your friends and neighbours have been sick with COVID this summer, you are not wrong.Ottawa is experiencing a COVID-19 wave that is sending people to hospital, causing outbreaks in long-term care homes, retirement homes and hospital wards, and even causing deaths among some of the most vulnerable. At least one local hospital has tightened masking requirements following outbreaks there, and Ottawa Public Health is advising students to take precautions when they head back to school, including staying home when sick and wearing masks for their own protection and the protection of others.
Advertisement 2
Story continues below
Trending
-
High rates of COVID are causing outbreaks, rising hospitalizations and deaths heading into the school year

-
Slain Ottawa woman remembered as loving mother, amazing friend and motorsport enthusiast

-
Federal government to use 22 properties in Ottawa for housing

-
Murder charge laid in alleged 'femicide'

-
Ottawa woman dead following head-on collision on Highway 7 near Perth

Health Canada, meanwhile, is expediting its review of three updated vaccines that target the variants driving the current surge.
Relatively high rates of COVID seem likely to continue into the school year which comes during a period of increased fall social activity — a recipe for even more spread.
According to the most recent data from Ottawa Public Health, at least six Ottawa residents died of COVID-19 during the first part of August. Seven people died in July. During the week ending Aug. 18, 44 people were admitted to local hospitals with COVID-19 and there were 15 new and 11 ongoing COVID-19 outbreaks in Ottawa long-term care homes, retirement homes and hospitals, a number considered high. Eighty-two per cent of people admitted to hospital with COVID-19 were over the age of 60.
Unlike most communities in Ontario, Ottawa continues to track the virus that causes COVID-19 through wastewater. The Ontario government stopped funding the province’s internationally recognized wastewater surveillance program as of the end of July. Ottawa is one of just a small handful of communities that is continuing to track wastewater, for now. Extended funding for Ottawa’s wastewater surveillance program runs out at the end of September.
Advertisement 3
Story continues below
Article content
For now, that gives Ottawa Public Health officials a more accurate look at the amount of COVID-19 circulating in the community. Wastewater readings, which are at levels not seen since last winter, can serve as an early indicator for possible outbreaks. At a time when few people are being tested, wastewater surveillance, along with hospitalizations and outbreak numbers, provides a snapshot of the level of COVID-19 in the community.
And in Ottawa right now, it is high — not near the peak last winter, but continuing to spread.
Unlike many other respiratory illnesses, COVID-19 is not seasonal. Summer waves, generally smaller than fall or winter waves, have been a feature throughout the pandemic. But this year’s is bigger than most in some parts of North America.
The summer COVID wave is being driven by new variants known as FLiRT (named after technical names for their mutations). In the U.S., some states are seeing the highest summer surges of COVID-19 in years. Surges in infections led to the recent closure of two schools, one in Alabama and one in Tennessee, which returned to remote learning.
Advertisement 4
Story continues below
Article content
The new variants “have an extraordinary ability to bypass previous immunity,” said uOttawa epidemiologist Raywat Deonandan. They don’t necessarily make people sicker, but they have the ability to infect more people, which represents a threat to those who are most vulnerable to more severe outcomes from COVID-19 infections.
The wave comes at a time when just 23 per cent of Ottawa residents have received a COVID-19 vaccine since last September. The vast majority of people under the age of 60 have not been vaccinated in the past year. Vaccination rates are as high as 69 per cent for older residents, nowhere near earlier vaccination rates. Many people, though, have an added layer of immunity from previous infections.
The Ontario government offered a limited vaccination rollout last spring for older adults and those with compromised immune system. The planned fall vaccination campaign will include updated vaccines for the general population.
Last week, amid a substantial summer surge that is infecting more than one million people a day according to some models, the U.S. Food and Drug Administration approved updated mRNA COVID-19 vaccines that more closely target the circulating virus strains than previous vaccines. Those vaccines are expected to begin rolling out in a matter of days. The U.S. government will also begin distributing free COVID tests by mail beginning later in September.
Advertisement 5
Story continues below
Article content
Health Canada is reviewing submissions from Pfizer and Moderna for vaccines that target the KP.2 strain, according to a statement. It is also reviewing a submission from Novavax for a COVID-19 vaccine targeting the JN.2 strain. Those reviews are being done on an expedited timeline, said Health Canada spokesperson Anna Maddison. She said Health Canada is aiming to complete the review within 75-100 days, compared to the “performance standard” of 180 days. Pfizer and Moderna produce mRNA vaccines. Novavax is a traditional protein subunit vaccine, which some people prefer.
Health Canada says it will authorize the vaccines if, following an independent scientific review of the evidence, it determines they meet safety, quality and efficacy standards.
Given immunity from previous infections and vaccines, Deonandan of uOttawa said there is little sense that the current COVID-19 wave could “reach crisis levels” seen earlier in the pandemic when hospitals had difficulty coping.
“It is not the existential threat to society that it once was, but it is still a threat to lots of people, so we should take it seriously.”
Advertisement 6
Story continues below
Article content
He noted that many people feel they have already been vaccinated, but the virus that causes COVID-19 changes so frequently that updated vaccines are needed for protection.
“People don’t understand that COVID is in the top 10 list of killers in North America and globally, including in children.”
He said he struggles to understand why information about COVID-19 levels, from wastewater and elsewhere, is increasingly impossible to come by.
“The bottom line is if you are going to ask people to do their own risk management then give them the information they need.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,022
You might want to wait until fall for your next COVID-19 shot, doctors say. Here's why
Updated vaccines under review by Health Canada take aim at waning immunity, changes in virus

Amina Zafar · CBC News · Posted: Aug 28, 2024 4:00 AM EDT | Last Updated: 3 hours ago

Public health nurses are gearing up to get the latest vaccines to protect against severe COVID-19 into the arms of Canadians this fall. (Evan Mitsui/CBC)
Social Sharing
-
Facebook
-
X
-
Email
-
Reddit
-
LinkedIn
As COVID looms over the Paralympic Games in Paris that start Wednesday following outbreaks among Olympic athletes, new subvariants of Omicron continue to ebb and flow and make people ill. Doctors and public health experts want people to consider getting immunized as part of their fall plans.
Mandy Cohen, director of the U.S. Centers for Disease Control and Prevention, told reporters on Aug. 22 why officials think the updated vaccines are important.
"While the COVID virus continues to mutate and change faster than the flu virus, our underlying immunity from prior vaccines and prior infections provides some protection," Cohen said. "But we know that protection decreases over time, and certain groups continue to be at higher risk from COVID and other viruses, and we need to continue to protect ourselves and our loved ones."
Dawn Bowdish, an immunology professor at McMaster University in Hamilton, Ont., said COVID activity tends to peak every three to six months, such as in this coming winter.

People continue to test positive for COVID-19 on rapid home tests. (Carolyn Ryan/CBC)
What variants are in the upcoming vaccine?
Along with the Omicron subvariants currently circulating in Canada and the U.S., KP variants that are offshoots of Omicron started spreading rapidly around the world in late 2021.Vaccine makers and regulators like Health Canada are now gearing up to get the latest protection into arms.
"Health Canada is reviewing submissions from Pfizer and Moderna for COVID-19 vaccines that target the KP.2 strain," a spokesperson said on Tuesday. "We are also reviewing a submission from Novavax for a COVID-19 vaccine targeting the [earlier] JN.1 strain."
The regulator said it plans to "complete the review process by early autumn," with doses arriving days after.
WATCH | Why some doctors say you should wait:

Some doctors say wait until fall for your next COVID shot
9 hours ago
Duration 2:07
Despite high COVID-19 case counts, some doctors are advising their patients to wait until fall for their next shot. Health Canada is expected to finish its review of several new vaccines by then.
Who should wait to receive an updated vaccine?
Dr. Iris Gorfinkel, a family physician in Toronto, said some of her patients are already asking about a fall vaccine dose."The most common question by far and away is, 'Should I get my COVID vaccine now?'" Gorfinkel said. "Right now, because fall is around the corner, I'm recommending that they actually wait. Wait for that better-matched vaccine because chances are it's going to reduce hospitalization."
The shots aren't expected to perfectly match to circulating subvariants, she added, but they should reduce people landing in hospital.
Bowdish said older adults ask her all the time about COVID vaccinations. "They are really feeling left behind at not having good information."
Federal officials say Canada has "secured sufficient supply of COVID-19 vaccines to meet provincial and territorial requirements for fall and winter 2024 vaccination campaigns."
A fall vaccine could be an option for anyone concerned about maximizing protection over the winter holidays, U.S. officials said.

Updated COVID vaccines have been likened to recharging batteries of immune protection. (Evan Mitsui/CBC)
Who should get a jab right now?
Individuals who are 65 and older, people with underlying conditions, including obesity or heart or lung conditions, should get a fresh dose sooner if they were last vaccinated over six months ago, Gorfinkel advised. That's in line with vaccine recommendations from Canada's national advisory body."Anyone who's at high risk of hospitalization and who is more than six months out from a vaccine is probably better served by getting vaccinated, even if it's an imperfect match right now," Bowdish said.
The current vaccines available in Canada target XBB.1, an earlier subvariant of Omicron, that was first reported in August 2022, said Ontario health officials.
WATCH | Canada's new virus lab:

Canada building new lab to work with world's most dangerous pathogens
5 months ago
Duration 2:17
The new Level 4 lab at the University of Saskatchewan, which will contain the new Canadian Centre for Pandemic Research, is being developed as the federal government is working to improve biosafety and biosecurity measures for high-containment labs — and in the wake of security criticisms at Canada’s existing Level 4 lab in Winnipeg.
Why matching matters
Unlike with the influenza virus that causes flu, there are multiple seasons for COVID-19, including summer peaks.The virus that causes COVID-19 is not only changing, but our protection from past infection or immunization also wanes over time, health officials say.
That's why to get the best protection in season, updated vaccines are recommended.
"The only way you get long COVID is by having COVID," Dr. Peter Marks, vaccine chief for the U.S. Food and Drug Administration, told reporters.
- Masking returns to Laval hospitals as COVID-19 cases increase across Quebec
- Some Olympians test positive for COVID, but it's business as usual for many athletes
"With the new vaccine formulation coming for the fall, it's much like recharging your batteries and your protection for the upcoming winter season," Iqbal said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,023
Democrats and Republicans greet Covid spike with a collective shrug
“Any current debate on [Covid] is relatively meaningless,” said one pollster.
A Covid-19 test sign is displayed at a store as a pedestrian walks past in Chicago on March 11. | Nam Y. Huh/AP
By Adam Cancryn and Lisa Kashinsky
08/28/2024 05:00 AM EDT
Infections are running rampant after the Democratic confab in Chicago, with staffers on Vice President Kamala Harris’ campaign, reporters and other convention-goers all stricken — and in at least one case claiming the positive test was “worth it.” Cases also cropped up after the Republican National Convention in July.
And yet the single most-animating issue of the 2020 election is an afterthought for the major-party nominees coming out of two of the 2024 campaign’s biggest milestones — even as the virus remains an ever-present threat that’s shaped broader debates over key electoral issues like strength of the economy and the future of families’ health and child care.
Both campaigns have struggled with how — and how much — to address a pandemic that the U.S. never fully defeated, but that few Americans still want to dwell on.
Former President Donald Trump has bemoaned in speeches and interviews that he “never got the credit that we really deserved” for helping accelerate vaccine development in 2020, even as he later cast doubt on the shots’ importance and has more recently maneuvered to gain the backing of prominent vaccine critic Robert F. Kennedy Jr. and his supporters. Vice President Kamala Harris lauded President Joe Biden for bringing the pandemic “under control” when she took over his campaign but has hardly mentioned Covid since. Both parties have blamed the other for allowing deaths to spike under their watches.
‘Greatest comeback story never told’: Biden touts Covid relief efforts
“It’s very difficult to talk about politically, because it’s still present and neither side wants to acknowledge that this pandemic is still around,” said Matthew Bartlett, a Republican strategist and former Trump administration appointee with a background in global health.
But “if it continues to worsen,” Bartlett said, “both parties will be forced to address it.”
The rhetorical vacuum around Covid comes even as cases have surged over the summer, hospitalizing thousands and killing nearly 700 people in one week in late July. Though that is far less than during the height of the pandemic in 2020 and 2021, Covid still ranks as a top-10 cause of death — and more broadly, a disease capable of disrupting people’s everyday lives.
Yet Americans have never been less interested in the virus. Just a fraction of adults are seeking out new Covid vaccines each year, and even fewer wear masks or take the basic precautions that were once seen as standard.
“Voters do not like it being brought up at all,” said Celinda Lake, a Democratic strategist and pollster for Biden’s 2020 campaign, who marveled at the near-total absence of masks at a Democratic convention where roughly 20,000 people crammed into Chicago’s United Center for a week. “They want to get over it.”
With Covid receding from voters’ collective conscious — even as reports of post-convention cases keep coming — strategists posit it’s likely best for both candidates if talk of the pandemic fades away with it.
“Trump would be smart to just not talk about it,” said Mark Graul, a Wisconsin-based Republican consultant. And given the “relation” between the pandemic and the Biden-led economic recovery effort that voters now associate more with soaring inflation than rapid job growth, Graul said, “I’m not so sure it’s a smart move for [Harris] either.”
Lake, who has conducted focus groups across the battleground states, added that the only voters who bring up Covid now unprompted tend to be hardcore Trump supporters eager to bash the Biden administration’s response. And even those who might be inclined to side with Democrats on the issue prefer health care messaging that excludes mention of the pandemic.
Inside a Biden White House that has now reoriented itself around electing Harris, senior officials have continued to keep an eye on Covid, wary of a particularly dangerous flare-up during the key stretch of the election that could force the virus back into the public consciousness and damage Democrats politically.
But much of the day-to-day work has been shifted out of the White House and back to a Health and Human Services Department far less tied to political dynamics of the moment.
The Food and Drug Administration just approved updated Covid vaccines that are now rolling out widely. Those will be central to a just-launched fall campaign led by HHS called “Risk Less. Do More” encouraging people to get both their Covid booster and flu shot in tandem. The administration also plans to restart its distribution of free Covid tests at the end of September.
Biden and Harris, though, are not expected to play much of a public role in that effort, driven in large part by a recognition that most Americans mulling their vote ahead of November don’t want to hear about Covid — and a White House that has little desire to remind them.
“For most people, Covid is less about getting an infection and more about a period of time when our lives were super disrupted — and that is behind us,” said Ashish Jha, the Biden White House’s former Covid response coordinator. “We do still have a public health problem, but it is no longer in any way a substantive societal problem.”
White House spokesperson Kelly Scully touted the administration’s initial pandemic response as critical to ensuring that Covid “no longer meaningfully disrupts the way we live our lives,” while pointing to the ongoing efforts to manage the virus by making tests, vaccines and treatments widely available.
'That was painful for me': Fauci on correcting Trump during Covid
“When President Biden and Vice President Harris came into office, America was flat on its back reeling from a once-in-a-century pandemic with no plan from the previous administration to deal with Covid-19,” Scully said. “The Biden-Harris Administration took swift action to get America vaccinated — and get our economy and schools opened up.”


Responsible AI governance is good business
Sponsored ByIBM
Learn more
Yet two years removed from the pandemic’s crisis period, polling shows that Covid ranks far down the list of urgent voter priorities heading into November — if it shows up in surveys at all — with few Americans eager to revisit the painful memories of the pandemic era. The government has relaxed guidelines originally meant to limit the virus’ spread. And when Biden contracted Covid again in July, he did not wear a mask in public while actively shedding the virus.
During Biden’s abbreviated reelection run, he pointed to Covid as an example of the contrast in leadership between Trump and himself — accusing his predecessor of exacerbating a national crisis that he later said he successfully cleaned up. The president also highlighted the pandemic to show how much the economy had improved on his watch since then.
But that strategy never resonated with much of the electorate, and Harris has opted to take her campaign in a different direction by focusing almost exclusively on the future.
Fixating on the events of three years ago, aides and allies said, would risk distracting from the forward-looking campaign themes that have energized the electorate — and remind voters of the pinch they felt in their wallets from the inflation that grew out of the pandemic era.
But there is little benefit for Trump to harp on Covid, either. The Republican has long struggled to reconcile his messaging on Covid, torn between wanting credit for Operation Warp Speed, the program that accelerated developing the vaccine, and appealing to a base that distrusts mask and vaccine mandates and, in some cases, the very shot itself. He has recently attempted to play more into the latter, saying he would rehire military service members fired over Covid vaccine mandates “with an apology and with back pay” and threatening to withhold federal dollars from schools that require the jab.
“Any current debate on [Covid] is relatively meaningless,” said Democratic pollster Paul Maslin. “Each party cancels the other out.”

See how you can save up to USD 2.3 million on on-premises infrastructure spend annually
Sponsored ByIBM
Learn more
Harris’ campaign declined to comment while Trump’s campaign did not respond to an inquiry.
Still, the unpredictable nature of Covid — which is mutating more quickly than drugmakers can keep up with and is fueling surges outside of the typical winter period than infectious diseases experts initially predicted — could make it harder for Trump and Harris to ignore, especially if cases remain elevated as voting gets underway. Nearly one-third of respondents to a recent Axios-Ipsos poll said Covid poses a “large” or “moderate” risk to their health — an uptick from the same survey in early June, when cases were lower.
The “shock value” of each surge is more “muted” now that there are treatments and vaccines to prevent severe illness, Suffolk University polling director David Paleologos said.
But “as the virus spreads,” he added, “so will its importance in voters’ minds.”
Users who are viewing this thread
Total: 2 (members: 0, guests: 2)
Pakistan Defence Latest
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (7 Viewers)
- Latest: onlinpunit
-
-
-
-
Country Watch Latest
-
-
Iran Cyber Security and Artificial Intelligence (civilian and military) (2 Viewers)
- Latest: Immortals
-
-
-
Latest Posts
-
-
-
Iran Cyber Security and Artificial Intelligence (civilian and military) (2 Viewers)
- Latest: Immortals
-
New submarine detector shows ‘tremendous potential’ in South China Sea tests (4 Viewers)
- Latest: Beijingwalker
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (7 Viewers)
- Latest: onlinpunit
