Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #292
Alberta is bringing in more rapid COVID-19 tests as millions destined to be tossed
At least 25 million individual rapid tests set to expire in March

Jennifer Lee · CBC News · Posted: Feb 20, 2024 4:54 PM EST | Last Updated: 4 hours ago

Millions of COVID-19 tests stored in an Alberta Health Services warehouse are set to expire on various dates through March. (Paul Smith/CBC)
Social Sharing
- X
According to Alberta Health, five million rapid antigen test kits, each containing at least five individual tests, are set to expire in March and will be discarded.
Another large stash of tests that expired Jan. 1 have already been tossed. In November, the province told CBC News that 760,000 boxes were in a central warehouse with that expiry date.
At Cambrian Pharmacy in Calgary, pharmacist Mathieu Giroux said that while demand is not nearly as high as it once was, he is still placing regular orders for rapid COVID tests.
But lately, some of his customers are choosing to wait when they realize the limited shelf life left on the current stock.
"Some people don't want them because the expiration is short," said Giroux.
They want to have them on hand, but since they're expiring in less than a few weeks or a month, they're just going to pass for now."
More tests coming
CBC News reached out to the province to find out what it plans to do once its stockpile is depleted."Alberta Health is currently working with the federal government to receive additional COVID-19 rapid antigen tests with longer expiry dates, ranging from September to December 2024," an Alberta Health spokesperson said in an email.
"The tests will begin arriving in Alberta [in the] next few weeks."
The shipments are expected to include the BTNX, Panbio, Artron and Roche brands.
According to the province, rapid tests will be provided free of charge through participating community pharmacies, until mid-December, as long as supplies last.

Dr. Nitika Pant Pai is an associate professor in the department of medicine at McGill University. (Nitika Pant Pai)
Dr. Nitika Pant Pai, who has studied the use of rapid antigen tests, is disappointed to hear so many tests have gone unused and will be discarded in Alberta.
"These could have been used in other parts of the world where there are no tests," said Pai, associate professor in the department of medicine at McGill University and a senior research scientist at the Research Institute of the McGill University Health Centre.
"This is wisdom in hindsight. Could we have done something better if we knew that they were expiring in six months? Could we have rolled them out … or given them away to other parts of the world where people are still suffering from COVID?"
Pai welcomes Alberta's decision to order more kits. But she said testing fatigue is a concern.
"All of us are tired of testing. But the good part about testing is that when you know you have symptoms and you get tested, you're actually empowering yourself to take the next best action plan."
That includes staying home when you are sick, which continues to prevent transmission and protect others, she said.
"At this point, it's a matter of responsibility. And that, I think, is very important and the messaging has to be clear about that," Pai said.
"It's always a good idea to be proactive, not just about your health, but public health. And those are the lessons that COVID has taught us."
Dr. Dan Gregson of the University of Calgary is not surprised by news that expired rapid tests will be discarded.
"I think that the government has tried to ensure that we have enough kits for people who want to do testing," said Gregson, an associate professor in the Cumming School of Medicine, specializing in infectious diseases and medical microbiology.
"And the uptake has been decreasing over time as the situation changes with regards to COVID."
According to Gregson, people who are symptomatic should still be staying home for the first five days of the illness.
Since the vast majority of Albertans are not eligible for costly PCR testing, which requires lab processing, Gregson believes there is still value in testing with a home kit.
"If it's going to change your behaviour — if you're going to say that 'if I test positive, I'm going to wear a mask after I'm at home for five days' — that's helpful."
Gregson said the rapid tests can also help higher risk Albertans, including those eligible for treatments such as Paxlovid.
"It gives you the option of testing at home and, if you're positive, not having to go through Health Link to get a PCR test done," he said, adding high-risk Albertans should follow up with a PCR test if their rapid test is negative.
He recommends swabbing both the nose and throat to increase sensitivity of the test.
And repeat testing is important, too, he said, because rapid tests can come back negative early in the illness when viral loads are low.
"You can improve your sensitivity by doing repeat testing over time — three or four times during that initial phase of your illness — to try and increase the sensitivity. But nothing's 100 per cent."
COVID-19 testing guidance can be found on the Alberta government website. Information on which pharmacies offer the free rapid COVID-19 tests can be found here.
"Albertans can also connect with their local pharmacy and ask them to order in no-cost rapid antigen tests from their pharmacy wholesaler to be made available," an Alberta Health spokesperson said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #295

Covid death toll in US likely 16% higher than official tally, study says
Researchers think undercounting goes beyond overloaded health systems to a lack of awareness of Covid and low levels of testing
Covid death toll in US likely 16% higher than official tally, study says
Researchers think undercounting goes beyond overloaded health systems to a lack of awareness of Covid and low levels of testingMelody Schreiber
Wed 21 Feb 2024 15.00 GMT
The Covid death toll in the US is likely at least 16% higher than the official tally, according to a new study, and researchers believe the cause of the undercounting goes beyond overloaded health systems to a lack of awareness of Covid and low levels of testing.
The second year of the pandemic also had nearly as many uncounted excess deaths as the first, the study found.
More than 1.1 million Americans have died from Covid, according to official records. But the actual number is assuredly higher, given the high rates of excess deaths. Demographers wanted to know how many could be attributed to Covid, and they drilled down to data at the county level to discover patterns in geography and time.
There were 1.2 million excess deaths from natural causes – excluding deaths from accidents, firearms, suicide and overdoses – between March 2020 and August 2022, the researchers estimated, and about 163,000 of those deaths were not attributed to Covid in any way – but most of them should have been, the researchers say.
Once they determined how many more people had died than expected, more questions arose.
“Everyone has wanted to know: why did all these extra deaths happen?” asked Elizabeth Wrigley-Field, associate professor in the department of sociology and the Minnesota Population Center at the University of Minnesota and one of the study’s authors.
To get closer to that answer, they first looked at when and where excess deaths occurred.
The researchers thought they might see the deaths happening at the peak of major surges or shortly thereafter, when health systems were overwhelmed and health workers were exhausted and sick themselves.
Instead, the excess deaths began ticking up in the month before, in the lead-up to major surges.
“The mortality that’s not considered Covid starts a little bit before the Covid surges officially start and crests a little bit sooner,” Wrigley-Field said.
That indicates some people didn’t realize their illness was Covid, due to a lack of awareness about its prevalence and low levels of testing. There was also a rise in out-of-hospital deaths – in homes and nursing homes, for instance – which makes ascertaining the cause of death more difficult.
The researchers also thought they would see under-reporting of Covid deaths mainly in the early months of the pandemic, as other research has indicated. It was still a novel virus then, and not everyone knew the symptoms or had access to tests.
“Quite the contrary, we find over the first 30 months of the pandemic that serious gaps remained in surveillance,” said Andrew Stokes, associate professor of global health and sociology at Boston University and one of the study’s authors.
“Even though we got a lot better at testing for Covid, we were still missing a lot of official Covid deaths” in the US, said Jennifer Dowd, professor of demography and population health at University of Oxford, who was not involved in this research.
The phenomenon “underscores how badly the US fared as the pandemic continued”, Wrigley-Field said. “It does profoundly reflect failures in the public health system.”
As for where the deaths occurred, “there was marked regional variation”, Stokes said. The hardest-hit were non-metropolitan counties, especially in the west and the south – areas that don’t have as many resources for investigating deaths, and which have had lower levels of testing for Covid, he said.
These differences are also likely explained by different state-level policies, how jurisdictions count Covid deaths, and the politicization of the crisis down to the local level, where beliefs about Covid may have influenced the cause of death listed on certificates.
“Every jurisdiction is doing this differently, and that’s why this is such a mess,” Stokes said.
The US needs to invest in more complete and timely mortality reporting, the experts agreed.
While Covid deaths have now declined from soaring heights seen earlier in the pandemic, the virus is still deadly. “If we really want to know the impact, yes, that Covid is continuing to have on mortality, we still need to look at this excess over time,” Dowd said.
“We probably will be using these numbers for lots of reasons to try to understand what went right and what went wrong with Covid – and how we can do better for the next pandemic,” she said.
Knowing mortality rates helps authorities allocate resources, including vaccines, treatments, and extra health workers, to the hardest-hit populations and regions, and it can help individuals make more informed decisions about taking precautions.
Understanding Covid’s true death toll – and elucidating the reasons for under-counting – is important for the current responses to infectious diseases as well as preparing for the next pandemic, the researchers said.
“What does it take to be able to respond to a disaster as it’s unfolding?” Wrigley-Field asked. “Where are the places that, when there was a crisis, really were not able to keep people alive?”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #298
COVID Tracker | Cases increase; Bridge discontinuing tracker | Bridge Michigan
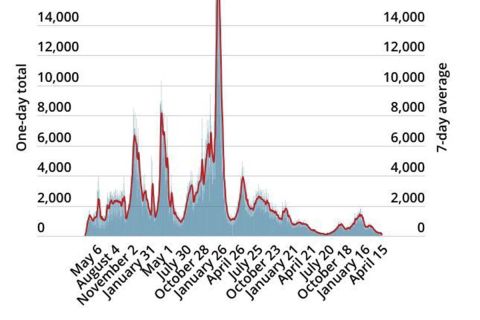
This tracker recorded Michigan's COVID-19 case numbers, positivity rate, county infection rates, and weekly cases along with maps and daily state curve data.
COVID Tracker | Pandemic deaths hit 39,999; weekly cases fall 9%
February 20, 2024Bridge Staff
Michigan Health Watch
Coronavirus Michigan
Last updated: Tuesday, Feb. 20, at 5:13 p.m. This post will be continuously updated with Michigan coronavirus locations and updated COVID-19 news.
For more interactive maps and charts, see the Michigan Coronavirus Dashboard, showing vaccine distribution information, case numbers, locations, deaths and demographics.
Michigan is approaching a grim milestone, with the state tally of confirmed COVID-19 deaths at 39,999 since the pandemic began in March 2020.
The number includes another 14 confirmed deaths during weekly reporting Tuesday. Last week, daily cases fell 9% to an average of 474 per day from 521 the preceding week.
Of the deaths, seven occurred in January and seven in February. So far in 2024, there have been 324 deaths.
Related: COVID-positive? Five-day isolation still recommended in Michigan
The state’s 164 hospitals reported 566 confirmed COVID-19 patients on Monday, down from the 601 reported a week earlier.
Experts say that state-confirmed cases are likely a vast undercount because many people either no longer test for the virus when they have symptoms or rely on home tests. Still, case counts are an indication of overall trends.— Mike Wilkinson
Tuesday, Feb. 13
Cases climb 7%
Confirmed COVID-19 cases last week climbed 7% to an average of 521 this week, up from 489 the week before, Michigan public health officials reported on Tuesday.It is the second consecutive week of increases after four weeks of declines.
The state also reported 19 additional COVID-19-positive deaths Tuesday, down from 227 a week ago. The vast majority of the deaths reported last week, 195, were in January and were reported later than usual.
Of the 19 reported Tuesday, 12 occurred in January, six in February and one in December. There have now been 310 confirmed deaths in 2024; there were 2,320 in all of 2023.
Related: Homeschool parents mobilize to fight Michigan efforts to add oversight
Seniors, and especially those over 80, are increasingly the most susceptible to COVID-19 fatalities, statistics show. Since the first week of December, 53% COVID-19 deaths in Michigan were those 80 or older, compared to 41% of the 39,173 deaths before then.
Those under 60 make up 14% of all deaths since the pandemic began in 2020 — but just under 8% of all deaths since December, a Bridge Michigan analysis of demographic data shows.
The state’s 164 hospitals reported 601 confirmed COVID-19 patients on Monday, up from the 569 reported a week earlier.
Experts say that state-confirmed cases are likely a vast undercount because many people either no longer test for the virus when they have symptoms or rely on home tests. Still, case counts are an indication of overall trends. — Mike
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #299

Do the latest vaccines better protect us from COVID-19?
For the first time, Australian researchers have sought to put a number on how much better newer vaccines shield us from severe disease.
Do the latest vaccines better protect us from COVID-19?

By Angus Dalton
February 20, 2024 — 7.50pmAs the federal government prepares to scrutinise how the COVID-19 pandemic was handled, a group of Australian scientists have fixed their sights on a crucial aspect of managing the virus in the future: the rollout of new vaccines.
They’ve analysed years of data to challenge a fundamental assumption: are newer vaccines actually better at protecting us against disease, especially when new variants easily outpace and outfox the rollout of new boosters?

Should we bother continually updating the vaccine?CREDIT:AP
This is the first analysis in the world to try to answer that question.
The results are fascinating, but there are important caveats – chief among them that the research is a pre-print, so it hasn’t been peer reviewed yet. Let’s take a look.
The vaccine-variant arms race
By the time a new COVID vaccine is tested, approved and released, invariably the immunogen used to create the vaccine – i.e. the spike protein it’s designed to replicate in the body – doesn’t match up with the dominant variant circulating in the community.“Things move on, the virus mutates very quickly,” says Associate Professor Deborah Cromer, lead author of the research and head of the Infection Epidemiology and Policy Analytics Group at the Kirby Institute at the University of NSW.
The XBB1.5 monovalent vaccine is the newest booster available in Australia. But XBB1.5 – the “Kraken” variant – reached the height of its power about a year ago. JN.1 is the variant now dominant in Australia, the US, France and India.
Taking a look at the variant distribution in NSW, you can see XBB1.5 occupies a tiny share of COVID-19 infections, whereas JN.1 is responsible for about three-quarters of infections.
If the rise of new variants continually outpaces new boosters, is there a benefit to updating the vaccines at all?
As Cromer says: “We want to balance the cost of updating a new vaccine – and what we’d have to pay vaccine manufacturers – with the potential benefit that’s going to be gained from it.”
Increasing protection
To pin down that benefit, Cromer and her colleagues drew on studies that compared the neutralisation titre – that is, the level of virus-busting antibodies in people’s blood – produced by different vaccines.“Once we accounted for all the obvious differences between the groups, there was still essentially a 40 per cent higher boost to neutralising antibody titres for every vaccine update,” Cromer says.
That’s a 40 per cent greater antibody response from each new vaccine. And that improvement applies across different COVID strains we’re exposed to – not just the specific variant a person has been immunised against.
However, a 40 per cent increase in neutralisation titre doesn’t automatically translate into 40 per cent better protection against symptomatic and severe disease.
In previous data analyses, Cromer and her colleagues established a quantitative relationship between the level of neutralising antibodies in the blood and protection from COVID.
They drew on this relationship to predict the effect that a 40 per cent increase in antibodies would have on clinical outcomes.
An updated booster, they estimate, would provide 11-25 per cent better protection against symptomatic disease and 23-33 per cent better protection against severe disease, compared to an older booster.
How do the numbers stack up?
So how impressive is that uptick in booster power? It depends which way you look at it.“There is definitely a benefit of continually updating the vaccine, which wasn’t necessarily what I was expecting to see,” Cromer said.
“But I also think that benefit is relatively small, perhaps smaller than some people might have hoped. You’d never normally licence a vaccine based on 20-30 per cent effectiveness. Therefore, the speed with which we rush into using these new vaccines should be balanced with potential costs.”

Facilities that can producce mRNA vaccines – such as BioNTech’s modular ‘Biontainer’ which will be installed in Victoria – could speed up the development and release of new vaccines.
For Associate Professor Paul Griffin, an infectious disease expert at the University of Queensland who wasn’t involved in the study, the findings underscore the benefits of faster vaccine rollout.
“Forty per cent is a useful improvement,” Griffin says. “But it’s likely the improvement could’ve been greater if there weren’t delays in rolling out those vaccines.”
He said a quicker regulatory process, the capacity to manufacture RNA vaccines in Australia, and better-designed vaccines that include multiple variants, would improve future boosters’ ability to protect people.
Chair of epidemiology at Deakin University, Professor Catherine Bennett, points out the study’s 40 per cent finding has a wide confidence interval – statistical guardrails around the final estimate. While 40 per cent is the researchers’ best guess, the actual improvement between each vaccine could be as low as seven per cent or as high as 82 per cent.
“It might be an even stronger effect, or it might be a lesser effect – there isn’t the precision in this study to show it,” she says. “But what it is showing is … that you do get this better neutralising response with the more recent vaccines.”
While the pattern of strengthening vaccine effectiveness is welcome, we don’t know exactly why it’s reliably increased, given the mismatch between vaccines and variants. And the pattern may not last forever.
In any case, Cromer says, if you’re in a vulnerable demographic and you’re due for a booster, don’t wait for a new vaccine formula. People who are up-to-date with a recent booster are less likely to have severe symptoms, end up in hospital, infect others or contract long COVID.
“It’s much more important to get vaccinated than to get vaccinated with the latest variant.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #300

Opinion: COVID is still with us, so go get vaccinated
Only 18 per cent of Quebecers have received the latest booster — while cases and hospitalizations mount in Montreal and globally.
Opinion: COVID is still with us, so go get vaccinated
Only 18 per cent of Quebecers have received the latest booster — while cases and hospitalizations mount in Montreal and globally.Author of the article:
Mariane Saroufim • Special to Montreal Gazette
Published Feb 21, 2024 • 3 minute read

Article content
We all remember when the COVID-19 pandemic was at its peak — the lockdowns, the restrictions, the daily death count. After the vaccination campaigns, it was easy to believe we had entered a post-COVID world. Unfortunately, that is not the case.With new cases rapidly increasing in Montreal and globally, and the old vaccines no longer offering complete protection, it is important for all of us to get the latest booster to protect ourselves and those around us.
The latest Omicron subvariant — known as JN.1 — started circulating in the fall and demonstrated that COVID-19 is still very much present. Yet vaccination numbers show abysmally low adherence to the most recent recommendations by Quebec health authorities.
Since the beginning of the fall immunization campaign — meant to prepare for winter COVID-19 surges — only 17.8 per cent of Quebecers received the latest booster protecting against all variants, including JN.1.
Meanwhile, COVID-19 cases have increased rapidly in Montreal and globally.
According to the World Health Organization, the number of new COVID-19 cases and hospitalizations have been rising globally by four per cent and 40 per cent, respectively, from Dec. 11, 2023, to Jan. 7, 2024, compared to the previous 28-day period.
In the U.S., an estimated 35,000 people were hospitalized with COVID-19 during the last week of December.
Moreover, JN.1 is spreading rapidly through the Quebec population. While the proportion of COVID-19 cases attributable to JN.1 was 45 per cent in early December, it had increased to 93 per cent by the end of January. This rapid spread is in part due to the low number of vaccinated people, in addition to the virus being different enough that our immune system doesn’t recognize it as well.
Beyond the symptoms, the new variant is a cause for concern because the combination of rising flu, RSV and COVID-19 cases places an increased burden on our health-care system. “When you look at the numbers across the province, you’re seeing that the emergency rooms everywhere are very full,” noted Dr. Christopher Labos, epidemiologist, cardiologist and Gazette contributor.
The National Advisory Committee on Immunization (NACI) and Quebec’s Ministry of Health and Social Services are specifically recommending boosters for all persons who are 65 and older, those living in long-term care homes or seniors’ homes, and those who are six months or older and immunocompromised.
However, the general population is also eligible and should get vaccinated. A single dose of the new vaccine is sufficient for a person to be considered adequately protected.
As a community, Montrealers must take care of each other. Getting the latest booster helps protect vulnerable members of the community, slow the spread of new variants, lower the chances of serious illness, hospitalization and long-COVID symptoms, and reduce the burden on our health-care network.
Let’s not allow the spread of COVID-19 to become normalized. Get your vaccine (Moderna or Pfizer-BioNTech) at your nearest Integrated University Health and Social Services Centre (CUISSS) with or without an appointment.
Users who are viewing this thread
Total: 2 (members: 0, guests: 2)
Pakistan Defence Latest
-
-
-
-
-
Reports: Bajwa agreed to curtail Pakistan’s ballistic missile program (4 Viewers)
- Latest: SteppeWolff
