Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #332

Moderna will supply COVID-19 vaccines made in Laval by fall 2025
The plant, whose construction was just completed, will be able to produce 100 million doses of mRNA vaccines annually, not just for COVID-19.
Moderna will supply COVID-19 vaccines made in Laval by fall 2025
The plant, whose construction was just completed, will be able to produce 100 million doses of RNA vaccines annually, and not only for COVID-19.Author of the article:
La Presse Canadienne
Stéphane Rolland
Published Feb 23, 2024 • 1 minute read

Moderna chief executive Stéphane Bancel, right, and Federal Industry Minister François-Philippe Champagne, left, tour the company's soon to open vaccine production facility in Laval on Friday, Feb. 23, 2024. PHOTO BY RYAN REMIORZ /The Canadian Press
LAVAL — A new Moderna plant in Laval will be able to supply COVID-19 vaccines for the fall 2025 vaccination campaign, the company said Friday during an official visit to mark the end of construction work at the messenger RNA production facility.
The $250-million Laval plant should produce about 100 million doses of RNA vaccines annually, “able to provide vaccines to all Canadians,” said Moderna’s chief operating and quality officer, Jerh Collins.
In April 2022, the federal government reached an agreement with Moderna to set up a factory in Quebec. The choice of Laval was revealed in August 2022 and work was launched in November 2022.The factory will be able to do much more than produce vaccines against COVID-19, noted the minister of Innovation, Science and Industry, François-Philippe Champagne, at a news conference.
“Moderna is not just about COVID-19. This is a range of vaccines that we will be able to produce at home. … There are even vaccines potentially for cancer.”
Quebec’s economy minister, Pierre Fitzgibbon, emphasized the project makes it possible to reduce Canada’s dependence on foreign vaccine production.
He said Moderna’s new project will serve as a calling card to attract other projects in the pharmaceutical sector to Quebec.
“There are international pharmaceutical companies that are looking at what is happening, the talent that there is at McGill, that there is at Université de Montréal, among others. … I think it will create quite significant momentum for life sciences.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #333

COVID vaccines linked to many serious health-related issues
The most notable COVID vaccines, such as those developed by Pfizer-BioNTech and Moderna, employ various technologies
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #334
Senior dies of COVID-19, raising death toll to 11 this year in Waterloo Region
Hospitalizations for the disease are stable and relatively low.
Senior dies of COVID-19, raising death toll to 30 this year in Waterloo Region
Hospitalizations for the disease are stable and relatively lowByJeff Outhit Reporter
Friday, February 23, 2024
1 min to read
Article was updated 16 hrs ago

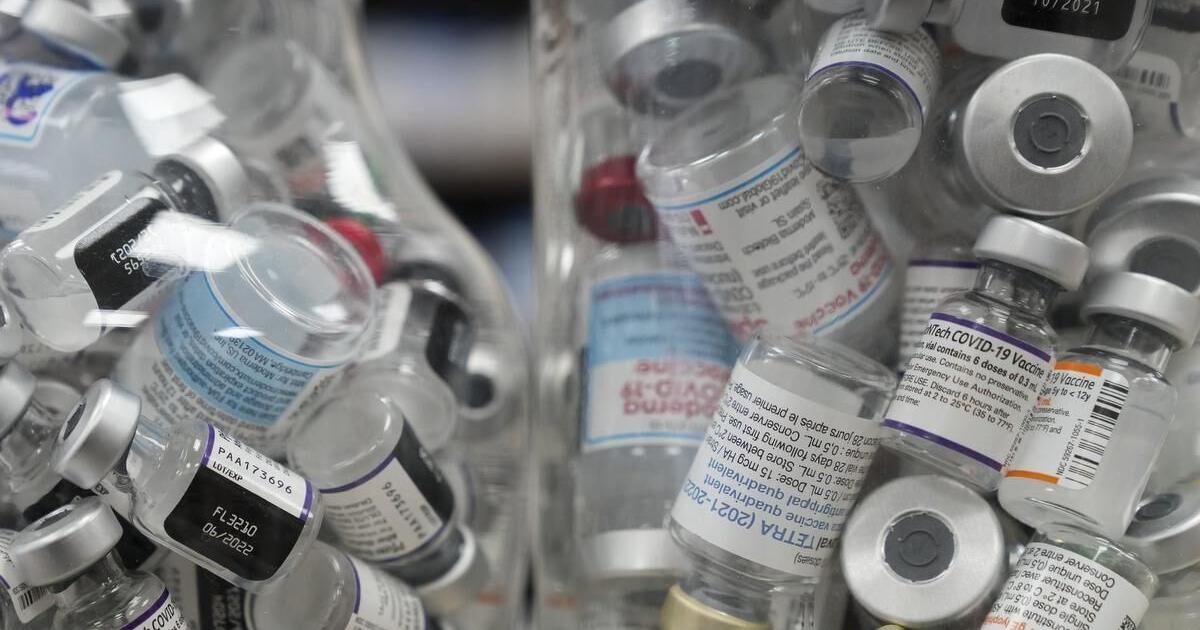
Jars full of empty COVID-19 vaccine vials.
Metroland file photo
A man in his 70s has died of COVID-19, the regional public health unit announced Friday in a weekly update.
This raises the death toll to 30 this year where the pandemic disease was a main or contributing cause.
Hospitalizations for the disease are stable and relatively low, averaging 13 patients per day on Feb. 17. This compares to a typical day in the pandemic with 27 patients in three local hospitals.
There is just one active COVID-19 outbreak in a high-risk setting, down from three outbreaks previously reported. It is in a nursing home.
Two other nursing homes in the region have active flu outbreaks, the first such outbreaks this year.
Sewage detection points to a pandemic virus that is at moderate levels in Kitchener and is trending downward in Cambridge.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #338

Covid inquiry: Doctor's anger at 'form of genocide' in care homes
Laura McClelland says the extent of the harms caused by Covid are yet to be fully appreciated.
www.bbc.com
Form of genocide in care homes during Covid - doctor
8 hours agoShare
Jenny ReesHealth Correspondent

Intensive care doctor Laura McClelland worked in one of the hospitals that bore the brunt of Covid cases in the early months of the pandemic
Discharging untested patients to care homes during the Covid-19 pandemic was "a form of genocide", a front-line doctor has said.
Intensive care doctor Laura McClelland said three things still made her angry four years on from the start of the pandemic.
She added doctors had little option but to discharge patients as they struggled to "rustle up" carers who were willing to risk their lives for minimum wage jobs.
She was speaking ahead of the UK Covid inquiry's three-week visit to Wales, which begins on Tuesday.

0:58
Covid: Discharging patients to care homes 'was genocide'
When the pandemic broke out, Dr McClelland was working at the Royal Gwent Hospital in Newport, one of those that bore the brunt of the first wave.
She also featured in a BBC Wales documentary made during that time.
She finds it difficult to talk about some of her experiences – the toll on staff, patients and loved ones is not easily forgotten.
And while she is proud of the sacrifices she and colleagues made to adapt and cope, her second source of anger is the impact it had on families, and those left grieving alone, under strict rules to minimise contact.
Trying to establish a rapport with relatives over a video link, as their loved ones were dying from Covid was "deeply inhuman for everybody involved," she said.
Establishing eye contact was near impossible as her visor meant all people saw were reflections bouncing off the plastic.
"I just have to hope the compassion got through," she said, recalling that even voices were muffled through the layers of PPE and background noise.
"It’s something I don’t think we will ever be able to get over".
Over the next three weeks the Covid inquiry will bring its hearings to Wales, focusing on the decisions made by the Welsh government.
Dr McClelland said accountability would be key for her.
"Sometimes we would invite patients’ families to be present via video call at the end of life - because people want to be there.
"And so I met many families for the first time via video call and was thrust into the reality of their loved one dying in the presence of strangers without them to hold their hand.
"We started using handprint kits more and taking locks of hair so that after a defined period of time those could be returned to the family - once they had been deemed to no longer be an infection risk."

Ann Richards' husband Eirwyn died from hospital-acquired Covid in January 2021
It was in stark contrast to the pre-Covid norm, when staff would come to know everything about a patient and their loved ones – with family photos and trinkets around the bed.
Infection-control measures – particularly in the early days of the pandemic – meant none of that was possible.
But not being able to say goodbye or see the body of their loved ones left many Covid-bereaved in an ongoing state of disbelief.
"For a long time I would pass the hospital and think 'is he still there?'" said Ann Richards, from Llandeilo, Carmarthenshire.
“Have they kidnapped him?” she laughed, recognising the absurdity of her question.
When her husband Eirwyn passed away in January 2021 she was told the news over the phone and was then unable to see his body at the funeral home.
"He died in a room on his own," she said.
"We weren’t allowed to see him and say our final goodbye. I know he’s gone, but we never had that final time together.
"He was put straight into a body bag and put into a coffin."
Eirwyn Richards was not able to have his family with him when he died
It is these unforeseen harms from decisions made during the pandemic that many hope will be addressed by the inquiry.
Dr McClelland said it was a familiar theme and she had encountered many bereaved relatives who still hoped there had been a mistake, simply because they were not there to witness the terminal decline first hand.
"This is a well-known psychological phenomenon and there are lots of people affected by this," she said.
"One gentleman would phone us every night to ask about his daughter and she'd died weeks and weeks before - he just wasn't able to be there at the end."
The harms from the choices made during that period are Dr McClelland’s third source of anger.
She is keen to hear decision makers explain why so much non-emergency healthcare was put on hold.
"I do think there is a great deal of anger within healthcare about the way that elective work was managed during that time," she said.
"Because it has now had such a significant impact and we are so far behind that we have let down hundreds of thousands of people - and therefore the true toll is still unfolding.
"We need to ask who is going to take true accountability for the impact that continues to have and that these decisions may very well have been the final nail in the coffin for the Welsh NHS."
There was also personal toll for those on the front line.
"We all put ourselves in the position of working within a high acuity Covid environment, knowing that we were surrounded by people who were dying and we could very well be next," she said.
"It was petrifying and we wondered whether we’d see our mums and dads again – whether we’d be there to raise our children.
"But we did what we had to do – thankfully, most of us did OK, but not everybody.
"We lost lots of colleagues who were doing exactly the same thing, but they had risk factors or were just extremely unlucky and they lost their lives caring for patients."
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #339

New Research Reveals High Prevalence Of Persistent COVID Infections - Health Policy Watch
A much higher percentage of the population has experienced “persistent” COVID-19 infections lasting more than 30 days than initially assumed, according to new
New Research Reveals High Prevalence of Persistent COVID Infections
COVID-19 26/02/2024 • Maayan Hoffman

A much higher percentage of the population has experienced “persistent” COVID-19 infections lasting more than 30 days than initially assumed, according to new research by the University of Oxford.
The study, published on February 21 in Nature, found that one to three of every 100 infections may last a month or longer.
The scientists, using data from the Office for National Statistics COVID Infection Survey (ONS-CIS), found 381 individuals with the same viral infection for a month or longer – including 54 whose persistent infection lasted two months and two over six months – out of 77,561 infections detected through ONS-CIS between November 2020 and August 2022.
In some cases, the infecting lineage had gone extinct in the general population. More than 90,000 ONS-CIS participants were sampled monthly for almost three years.
What “we uncovered is striking, given the leading hypothesis that many of the variants of concern emerged wholly or partially during long-term chronic infections in immunocompromised individuals,” the authors wrote in their paper. “As the ONS-CIS is a community-based surveillance study, our observations suggest that the pool of people in which long-term infections could occur, and hence potential sources of divergent variants, may be much larger than generally thought.”
In other words, the study debunks an assumption that new variants are only formed because of prolonged COVID-19 infections in immunocompromised individuals. This new study shows that the prevalence of persistent COVID-19 infections in the general population may be much higher and, therefore, also play a role in the evolution of the virus.
Persistence and Long COVID
Relatedly, the authors found that people with persistent infections lasting for 30 days or longer were 55% more likely to report having long COVID than people with more typical infections.“Although the link between viral persistence and Long COVID may not be causal, these results suggest persistent infections could contribute to the pathophysiology of long COVID,” said Co-lead author Dr Katrina Lythgoe of Oxford’s Department of Biology and its Pandemic Sciences Institute.
The paper carefully points out that not every persistent infection can lead to long-term COVID-19, and not all cases of long-term COVID-19 are due to persistent infection. “Indeed,” said Lythgoe, “many other possible mechanisms have been suggested to contribute to Long COVID, including inflammation, organ damage, and micro thrombosis.”
Nonetheless, “these results suggest that persistent infections could be contributing to the pathophysiology of long COVID,” the paper reads.

Mutation Rates
What about the rate of mutation?Some people who developed persistent infections had many mutations, suggesting they could act as reservoirs to seed new variants of concern. However, this was only sometimes the case.
“Certain individuals showed an extremely high number of mutations, including mutations that define new coronavirus variants, alter target sites for monoclonal antibodies, and introduce changes to the coronavirus spike protein,” the authors wrote. “However, most individuals did not harbour a large number of mutations, suggesting that not every persistent infection will be a potential source for new concerning variants.”
However, co-lead author Dr. Mahan Ghafari of Oxford’s Pandemic Sciences Institute in its Nuffield Department of Medicine, cautioned that the data from ONS-CIS did not include details about the medical history of people with persistent infections, so it was unknown how many of them were immunocompromised, such as with cancer, advanced HIV, etc.
He said the hope is that there would be further studies to better understand these individuals who developed persistent COVID and their health implications, and also to better understand how likely it is for these persistent infections to transmit highly mutated variants to the rest of the population.
Variant Reinfections
Finally, the scientists also found rare infections with the same variant. They identified only 60 reinfections by the same major lineage, suggesting that infection does build at least some immunity in infected individuals from the same variant.“Our observations highlight the continuing importance of community-based genomic surveillance both to monitor the emergence and spread of new variants, but also to gain a fundamental understanding of the natural history and evolution of novel pathogens and their clinical implications for patients,” Ghafari said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #340

Covid-19 update: 6084 new cases, 20 deaths
There were more than 200 people in hospital with the virus as of midnight on Sunday.
Covid-19 update: 6084 new cases, 20 deaths
about 1 hour ago
Of the new cases, more than half are reinfections. Photo: 123rf.com
The number of Covid-19 cases reported in the past week is down slightly compared to the week before.
There were 6084 cases in the week to midnight on Sunday, compared to 6312 in the week to 19 February.
Twenty deaths were attributed to the virus in the past week.
Of the new cases, 3935 were reinfections.
Canterbury was the region with the most reported cases, with 804, followed by Waitematā with 757 and Counties Manukau with 620.
There were 205 people in hospital with Covid as of midnight Sunday.
The number of cases in intensive care units was not available on the Te Whatu Ora website.
The seven-day rolling average of new cases was 868, down from 901 the week before.
ESR data last week showed the level of the virus in wastewater had risen for three weeks in a row.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #341
Weekly case numbers from around Australia: 7,350 new cases ( 1%), 1,310 hospitalised, 6 in ICU
1%), 1,310 hospitalised, 6 in ICU
Australia: Case Update
- NSW 2,401 new cases (
 2%); 800 hospitalised
2%); 800 hospitalised - VIC 723 new cases (
 3%); 156 hospitalised; 4 in ICU
3%); 156 hospitalised; 4 in ICU - QLD 1,508 new cases (
 6%); 292 hospitalised
6%); 292 hospitalised - WA 267 new cases (
 6%); 29 hospitalised
6%); 29 hospitalised - SA 1,549 new cases (
 1%); N/A hospitalised
1%); N/A hospitalised - TAS 724 new cases (
 12%); 13 hospitalised; 1 in ICU
12%); 13 hospitalised; 1 in ICU - ACT 105 new cases (
 44%); 20 hospitalised; 1 in ICU
44%); 20 hospitalised; 1 in ICU - NT 73 new cases (
 5%); 0 hospitalised
5%); 0 hospitalised
- Older more detailed surveillance reports can be accessed using the state and territory links above.
- These case numbers are only an indicator for the current trends as most cases are unreported.
- Multiply by 20 or 30 to get a better indication of actual community case numbers.
- NSW, VIC, QLD, WA and the ACT no longer collect or report RAT results.
Flu tracker tracks cold and flu symptoms (fever plus cough) and is another useful tool for tracking the level of respiratory viruses in the community.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #342
Early COVID-19 research is riddled with poor methods and low-quality results − a problem for science the pandemic worsened but didn’t create
Pressure to ‘publish or perish’ and get results out as quickly as possible has led to weak study designs and shortened peer-review processes.
 theconversation.com
theconversation.com
Early in the COVID-19 pandemic, researchers flooded journals with studies about the then-novel coronavirus. Many publications streamlined the peer-review process for COVID-19 papers while keeping acceptance rates relatively high. The assumption was that policymakers and the public would be able to identify valid and useful research among a very large volume of rapidly disseminated information.
However, in my review of 74 COVID-19 papers published in 2020 in the top 15 generalist public health journals listed in Google Scholar, I found that many of these studies used poor quality methods. Several other reviews of studies published in medical journals have also shown that much early COVID-19 research used poor research methods.
Some of these papers have been cited many times. For example, the most highly cited public health publication listed on Google Scholar used data from a sample of 1,120 people, primarily well-educated young women, mostly recruited from social media over three days. Findings based on a small, self-selected convenience sample cannot be generalized to a broader population. And since the researchers ran more than 500 analyses of the data, many of the statistically significant results are likely chance occurrences. However, this study has been cited over 11,000 times.
A highly cited paper means a lot of people have mentioned it in their own work. But a high number of citations is not strongly linked to research quality, since researchers and journals can game and manipulate these metrics. High citation of low-quality research increases the chance that poor evidence is being used to inform policies, further eroding public confidence in science.
Methodology matters
I am a public health researcher with a long-standing interest in research quality and integrity. This interest lies in a belief that science has helped solve important social and public health problems. Unlike the anti-science movement spreading misinformation about such successful public health measures as vaccines, I believe rational criticism is fundamental to science.The quality and integrity of research depends to a considerable extent on its methods. Each type of study design needs to have certain features in order for it to provide valid and useful information.
For example, researchers have known for decades that for studies evaluating the effectiveness of an intervention, a control group is needed to know whether any observed effects can be attributed to the intervention.
Systematic reviews pulling together data from existing studies should describe how the researchers identified which studies to include, assessed their quality, extracted the data and preregistered their protocols. These features are necessary to ensure the review will cover all the available evidence and tell a reader which is worth attending to and which is not.
Certain types of studies, such as one-time surveys of convenience samples that aren’t representative of the target population, collect and analyze data in a way that does not allow researchers to determine whether one variable caused a particular outcome.
Systematic reviews involve thoroughly identifying and extracting information from existing research.
All study designs have standards that researchers can consult. But adhering to standards slows research down. Having a control group doubles the amount of data that needs to be collected, and identifying and thoroughly reviewing every study on a topic takes more time than superficially reviewing some. Representative samples are harder to generate than convenience samples, and collecting data at two points in time is more work than collecting them all at the same time.
Studies comparing COVID-19 papers with non-COVID-19 papers published in the same journals found that COVID-19 papers tended to have lower quality methods and were less likely to adhere to reporting standards than non-COVID-19 papers. COVID-19 papers rarely had predetermined hypotheses and plans for how they would report their findings or analyze their data. This meant there were no safeguards against dredging the data to find “statistically significant” results that could be selectively reported.
Such methodological problems were likely overlooked in the considerably shortened peer-review process for COVID-19 papers. One study estimated the average time from submission to acceptance of 686 papers on COVID-19 to be 13 days, compared with 110 days in 539 pre-pandemic papers from the same journals. In my study, I found that two online journals that published a very high volume of methodologically weak COVID-19 papers had a peer-review process of about three weeks.
Publish-or-perish culture
These quality control issues were present before the COVID-19 pandemic. The pandemic simply pushed them into overdrive.Journals tend to favor positive, “novel” findings: that is, results that show a statistical association between variables and supposedly identify something previously unknown. Since the pandemic was in many ways novel, it provided an opportunity for some researchers to make bold claims about how COVID-19 would spread, what its effects on mental health would be, how it could be prevented and how it might be treated.
Many researchers feel pressure to publish papers in order to advance their careers. South_agency/E+ via Getty Images
Academics have worked in a publish-or-perish incentive system for decades, where the number of papers they publish is part of the metrics used to evaluate employment, promotion and tenure. The flood of mixed-quality COVID-19 information afforded an opportunity to increase their publication counts and boost citation metrics as journals sought and rapidly reviewed COVID-19 papers, which were more likely to be cited than non-COVID papers.
Online publishing has also contributed to the deterioration in research quality. Traditional academic publishing was limited in the quantity of articles it could generate because journals were packaged in a printed, physical document usually produced only once a month. In contrast, some of today’s online mega-journals publish thousands of papers a month. Low-quality studies rejected by reputable journals can still find an outlet happy to publish it for a fee.
Healthy criticism
Criticizing the quality of published research is fraught with risk. It can be misinterpreted as throwing fuel on the raging fire of anti-science. My response is that a critical and rational approach to the production of knowledge is, in fact, fundamental to the very practice of science and to the functioning of an open society capable of solving complex problems such as a worldwide pandemic.Publishing a large volume of misinformation disguised as science during a pandemic obscures true and useful knowledge. At worst, this can lead to bad public health practice and policy.
Science done properly produces information that allows researchers and policymakers to better understand the world and test ideas about how to improve it. This involves critically examining the quality of a study’s designs, statistical methods, reproducibility and transparency, not the number of times it has been cited or tweeted about.
Science depends on a slow, thoughtful and meticulous approach to data collection, analysis and presentation, especially if it intends to provide information to enact effective public health policies. Likewise, thoughtful and meticulous peer review is unlikely with papers that appear in print only three weeks after they were first submitted for review. Disciplines that reward quantity of research over quality are also less likely to protect scientific integrity during crises.

Rigorous science requires careful deliberation and attention, not haste. Assembly/Stone via Getty Images
Public health heavily draws upon disciplines that are experiencing replication crises, such as psychology, biomedical science and biology. It is similar to these disciplines in terms of its incentive structure, study designs and analytic methods, and its inattention to transparent methods and replication. Much public health research on COVID-19 shows that it suffers from similar poor-quality methods.
Reexamining how the discipline rewards its scholars and assesses their scholarship can help it better prepare for the next public health crisis.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #343

Remote instructor wins fight against Fanshawe College over COVID policy
A labour arbitrator has ruled against Fanshawe College in a dispute with a remote instructor over its COVID-19 vaccination policy.
Remote instructor wins fight against Fanshawe College over COVID policy
A labour arbitrator has ruled against Fanshawe College in a dispute over its COVID-19 vaccination policy for staff, finding a move to enforce the rule against a fully remote worker was unreasonable.Author of the article:
Jennifer Bieman
Published Feb 26, 2024 • Last updated 1 hour ago • 2 minute read

A labour arbitrator has ruled against Fanshawe College in a dispute over its COVID-19 vaccination policy for staff, finding a move to enforce the rule against a fully remote worker was unreasonable.
The Labour Arbitration Awards decision sided with Ontario Public Service Employees Union (OPSEU) Local 110, which had launched a grievance on behalf of Andy Wing, a full-time instructor in the college’s technical systems analysis program at its London campus.
“The college has not provided sufficiently cogent evidence that its interests in providing education to its students was outweighed in this case by the grievor’s (Wing’s) interest in his bodily integrity,” the Feb. 20 decision by arbitrator Larry Steinberg said.
The provincial government in August 2021 required all Ontario post-secondary institutions to draft and implement COVID-19 vaccination policies for staff and students. Fanshawe announced its policy in late September, the decision said.
Wing notified the college in October he had no intention of getting vaccinated and did not seek an exemption under Ontario’s Human Rights Code, the arbitrator’s ruling said. He was placed on a three-month unpaid administrative leave from Jan. 3 to March 7, 2022, for non-compliance with the policy, the decision said.
When Wing returned to work, he was placed on a non-teaching assignment for the rest of the 2022 school year before returning to teaching in September 2022, the decision said. Fanshawe’s staff vaccination policy was suspended in late April 2022.
The Fanshawe course, which Wing helped develop, was designed to be a fully remote program and launched in 2020, the decision said. Wing “had no need to be physically on campus” and there were no indications the structure of the program would be changing, the decision said.
“(Wing) had been working remotely for some time and carried out all of his duties including teaching and attending meetings with colleagues and students without any apparent difficulties,” the decision said.
The decision noted that in mid-December 2021, Fanshawe permitted students studying fully online who refused to provide proof of vaccination to submit a form declaring that they would not come to campus. No answer on why such a distinction was made was given in the proceedings, the decision said.
Fanshawe College declined comment Friday, saying the issue was a human resources matter.
Arbitration resolves disputes between employers and unions about the interpretation or application of the terms in a collective agreement. Grievance arbitration is a final and binding process.
The arbitrator’s decision left it to Fanshawe College and OPSEU Local 110 to determine an appropriate remedy. The exact details of the remedy were not immediately available.
OPSEU Local 110 president Mark Feltham was not available for comment Friday.
The arbitrator’s decision made it clear the union was not challenging any other aspect of the vaccination policy and said the outcome of the case was based on the specific facts of Wing’s situation.
“Different facts may very well result in a different outcome in respect of other employees working remotely,” the decision said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #344

Study reveals how long COVID can affect brain function through vascular disruption
The neurological response to coronavirus disease 2019 (COVID-19) may be due to brain-brain barrier (BBB) disruption.
Study reveals how long COVID can affect brain function through vascular disruption

By Pooja Toshniwal Paharia
Feb 26 2024
Reviewed by Lily Ramsey, LLM
In a recent study published in Nature Neuroscience, researchers investigated whether the neurological response to coronavirus disease 2019 (COVID-19) may be due to brain-brain barrier (BBB) disruption and subsequent extravasation of serum components.
 Study: Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment. Image Credit: fran_kie/Shutterstock.com
Study: Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment. Image Credit: fran_kie/Shutterstock.comBackground
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a respiratory viral infection resulting in severe acute respiratory distress syndrome (ARDS) and long-term neurological consequences such as headache, lethargy, malaise, and altered consciousness.BBB breakdown allows serum components and cytokines to penetrate the brain. The cerebrovascular pathophysiology and processes remain unknown, warranting further research.
About the study
The present study determined the association between COVID-19-related cognitive impairment and BBB breakdown in COVID-19 patients.The researchers collected blood and plasma samples from 76 acute COVID-19 patients, evaluated them for inflammatory, coagulation, and BBB dysfunction indicators, and rated their severity using World Health Organization (WHO) severity guidelines.
They next examined brain fog status to identify changes in patients' inflammatory profiles. During the first round of COVID-19 in March and April 2020, they recruited participants from St. James' Hospital at Trinity College in Dublin.
To investigate BBB function, the researchers selected ten recovered individuals, 11 suffering from long COVID or post-acute COVID-19 (PASC) and 11 with PASC-related brain fog, diagnosed with SARS-CoV-2 infection during the disease's April 2020 outbreak in Ireland.
All patients had polymerase chain reaction (PCR)-verified moderate-intensity COVID-19, requiring no antiviral therapy or hospitalization.
The researchers used the quick smell identification test (Q-SIT) to evaluate anosmia status, grouping them based on self-reported cognition difficulties known as brain fog.
They classified subjects as recovered in the case of no symptom recurrence after recovering from acute COVID-19. They used the Montreal Cognitive Assessment (MOCA) to measure cognitive impairment.
Oxygen Measurement eBook - Easily Understand Dissolved Oxygen Measurement eBook This ebook educates on basic information about dissolved oxygen (DO) measurement in a both brief yet understandable form.Download the latest edition
The researchers used dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) volume and thickness measurements on recovered individuals with PASC and 60 age-matched healthy controls from the IXI dataset to investigate structural brain alterations associated with increased BBB permeability.
They used multiplexed assays to assess 50 BBB integrity and inflammation markers and correlation analysis adjusting for age and sex to identify associations between neuroinflammatory and BBB dysfunction markers in the recovered and PASC cohort.
RNA-seq was also used to evaluate gene expression alterations in peripheral blood mononuclear cells (PBMCs) and the human brain endothelial cell line hCMEC/d3 isolated from unaffected, recovered, and patients with protracted COVID in the absence or presence of brain fog.
They used gene ontology (GO) to examine the transcriptome profiles of those with and without brain fog in the group with extended COVID.
The study included COVID-19 convalescents aged ≥18 years without neurological symptoms and individuals suffering from long-term COVID with symptoms lasting over 12 weeks after infection.
Results
COVID-19-induced brain fog was associated with BBB impairment. This disturbance is visible during acute COVID-19 and in individuals with long-term COVID-related cognitive impairment, popularly termed brain fog.In addition, the team found that PBMCs showed coagulation system instability and a suppressed adaptive immunological response in those with brain fogging.
In vitro, PBMCs showed enhanced adherence to cells of the human brain endothelium, whereas the endothelial cells were exposed to sera from individuals with prolonged COVID-19-induced inflammation.
The findings indicated that assessing BBB integrity might be a clinically helpful indicator of neurological sequelae linked with COVID-19 in a few individuals. Furthermore, targeted control of BBB integrity may provide a novel strategy for therapeutically treating patients with chronic COVID.
Common symptoms of brain fog include dyspnea, loss of smell and taste, coughing, weariness, and fever. Patients with brain fogging had a higher average age, were more likely to be hospitalized, and needed oxygen treatment.
There was a strong association between COVID-19 severity and age, hospitalization length, and comorbidities.
BBB failure was linked to long-term COVID-induced cognitive impairment, indicating that both active and acute SARS-CoV-2 infections may cause BBB dysfunction in individuals with neurological disabilities.
MRI imaging indicated significantly higher brain leakage in individuals with PASC and brain fog, with volumetric deficits mostly in the frontal and temporal lobes and increases in the occipital lobes and lateral ventricles.
White blood cells from COVID-19 patients stimulated brain endothelial cells. Compared to unaffected individuals, there were 950 differentially expressed genes (DEGs) in recovered individuals, 481 in individuals with protracted COVID, and 126 in those with brain fogging.
Upregulated genes were associated with T cell development and activation pathways, immune response negative control, and gene expression circadian regulation.
Conclusion
Overall, the study findings showed that PASC-related brain fog is associated with systemic inflammation and persistent localized BBB malfunction, with disruption apparent up to a year after infection.Dysregulation of the coagulation system is a primary cause of prolonged COVID-19. BBB disruption is associated with neurological impairment during acute COVID-19, and high serum levels in neurological diseases such as epilepsy, traumatic brain injury, and schizophrenia.
Understanding the long-term effects of COVID-19 is critical to developing new treatments.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #345
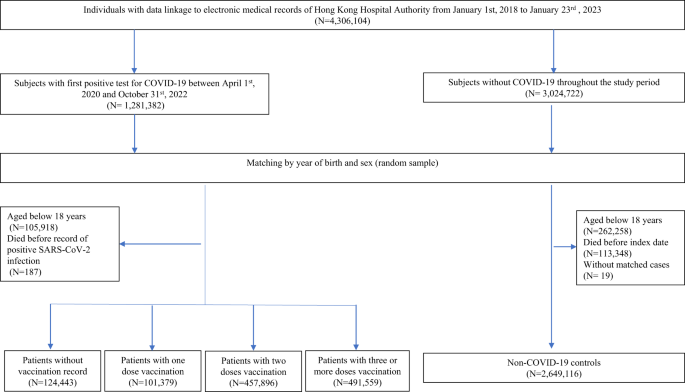
Persistence in risk and effect of COVID-19 vaccination on long-term health consequences after SARS-CoV-2 infection - Nature Communications
The long-term health consequences of COVID-19 infection are not fully understood. In this retrospective cohort study from Hong Kong, the authors describe changes in the risk of various clinical outcomes including all-cause mortality for one year following COVID-19 infection and how they vary by...
Users who are viewing this thread
Total: 2 (members: 0, guests: 2)
Pakistan Defence Latest
-
-
-
A GIDS Shahpar II UAV of the PAF broke midair and crashed near Darya Khan, Punjab (6 Viewers)
- Latest: studsmart
-
Israel and USA 'jammed GPS signals' in days before Iran's 300-missile launch to confuse attackers (3 Viewers)
- Latest: Cash gk
Country Watch Latest
-
Why India Deliberately kept Weakened Bangladesh’s Military | InShort (10 Viewers)
- Latest: AbuShalehRumi
-
-
Will the UAE reconsider the deal to purchase F-35 fighters with Trump’s possible return? (3 Viewers)
- Latest: Dalit
-
-
Not just engines, Tejas Mk-1A delivery could be hit over key Danish part, now on export blacklist (3 Viewers)
- Latest: silicon0000
Latest Posts
-
-
Why India Deliberately kept Weakened Bangladesh’s Military | InShort (10 Viewers)
- Latest: AbuShalehRumi
-
Afghan diplomats spark controversy by disrespecting Pakistan's national anthem (7 Viewers)
- Latest: SteppeWolff
-
-
