Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #835

How COVID-19 'breakthrough' infections alter your immune cells
New research from scientists at La Jolla Institute for Immunology (LJI) suggests people who received COVID-19 vaccines and then experienced "breakthrough" infections are especially well armed against future SARS-CoV-2 infections.
MAY 24, 2024
Editors' notes
How COVID-19 'breakthrough' infections alter your immune cells
by La Jolla Institute for Immunology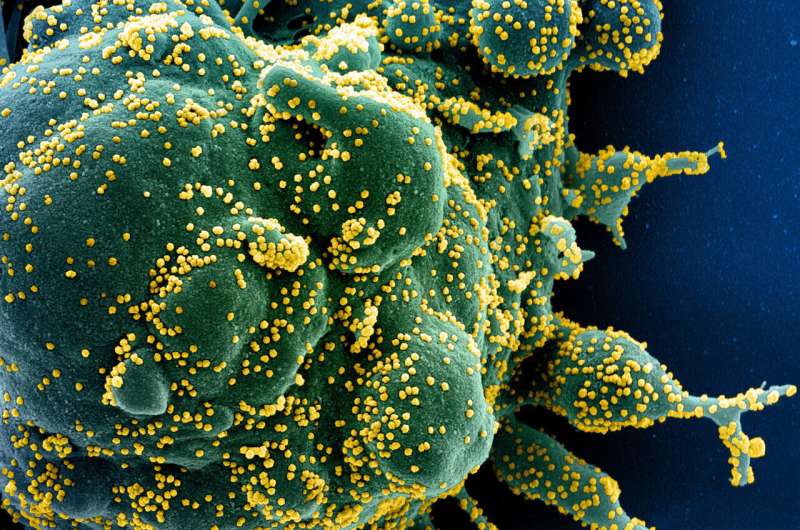
New research from scientists at La Jolla Institute for Immunology (LJI) suggests people who received COVID-19 vaccines and then experienced "breakthrough" infections are especially well armed against future SARS-CoV-2 infections.
By analyzing blood samples from study volunteers, the LJI researchers discovered that people who experienced symptomatic breakthrough infections develop T cells that are better at recognizing and targeting SARS-CoV-2, including the omicron and delta variants. The researchers describe this increased protection as an "immunity wall."
"The virus evolves, but, importantly, so does the immune system. T cells do not sit idle. Instead, they learn to recognize the parts of the virus that mutate," says LJI Professor Alessandro Sette, who co-led the Cell Reports Medicine study with LJI Professor Shane Crotty, Ph.D., and LJI Research Assistant Professor Alba Grifoni, Ph.D.
Study volunteers who experienced symptomatic breakthrough infections developed T cells that recognized multiple targets on the SARS-CoV-2 viral "Spike" and non-Spike epitopes. This infection left study volunteers with T cells that were better equipped to recognize mutated regions on new SARS-CoV-2 variants.
Even asymptomatic breakthrough infections boost T cell responses, though the effect was not as significant. Breakthrough infections also led B cells to produce cross-reactive antibodies against SARS-CoV-2. Most of these antibodies targeted the new viral variants and the original vaccine antigens.
The researchers found no evidence of harmful "T cell exhaustion" in study volunteers who had experienced repeated COVID-19 vaccinations and SARS-CoV-2 infections.
T cells gain fighting power
Many studies have shown that vaccination against SARS-CoV-2, the virus that causes COVID-19, provides people with significant immune protection against severe disease. Several LJI-led studies have shown that this immune protection is long-lasting and can even help protect the body from new viral "variants of concern."For the new study, LJI scientists investigated exactly how breakthrough infections affect T cells and B cells. The researchers followed a large group of study volunteers who had been vaccinated against SARS-CoV-2, the virus that causes COVID-19. Over time, many of these volunteers experienced breakthrough infections. The LJI scientists followed up with these volunteers to collect new blood samples post infection.
"With this study volunteer cohort, we were in a unique position to see how the immune system looked before and after a breakthrough infection," says Grifoni.
Study co-first author and LJI Postdoctoral Researcher Alison Tarke, Ph.D., spearheaded research showing that breakthrough infections prompted T cells to expand their "repertoires." That meant the cells could recognize multiple features, or antigens, on SARS-CoV-2.
These T cells appeared to develop their broad repertoires due to a combination of vaccination and breakthrough infection. COVID-19 vaccines taught the T cells to recognize a key part of SARS-CoV-2 called the "Spike" protein. Meanwhile, SARS-CoV-2 infection prompted T cells to recognize Spike, as well as several other viral proteins.
Breakthrough infection had left these study volunteers with T cells that could recognize and target SARS-CoV-2, even if part of it was mutated.
More layers of protection
Breakthrough omicron and delta variant infections also prompted B cells to produce more diverse antibodies. These antibodies could target epitopes that the vaccine and the infecting SARS-CoV-2 variant had in common.In fact, most of these new antibodies were good at attacking epitopes that the vaccine and the variants had in common. "New B cell responses that are only specific to the infecting variant, but not the vaccine, are very rare," says study co-first author and LJI Instructor Parham Ramezani-Rad, Ph.D.
The researchers uncovered another interesting trend in people with breakthrough infections. COVID-19 vaccines tend to be given in the upper arm, which means anti-SARS-CoV-2 immune cells develop far away from the upper respiratory system. SARS-CoV-2 tends to infect the upper respiratory tract first, which means there can be a delay getting the right immune cells to the scene of infection.
"A breakthrough infection has the potential of adding a layer of protection on top of a vaccine," says Grifoni.
What about asymptomatic infections?
As they worked, the scientists also found markers of previous SARS-CoV-2 infection in about 30% of study volunteers who had never shown COVID-19 symptoms. These volunteers appeared to have contracted asymptomatic cases of COVID-19 at some point earlier in the pandemic."Our study suggests most people who never thought they got a breakthrough infection actually did," says Grifoni. "The majority of the population appears to be affected by a combination of vaccination and one or more breakthrough infections."
No evidence of T cell exhaustion
The new study also addresses concerns that repeated infection or COVID-19 vaccine might lead to a phenomenon called T cell exhaustion, where T cells lose their ability to target a pathogen.The researchers discovered that breakthrough infections prompted T cells to produce more types of cytokines, signaling molecules that help fight infection. Before a breakthrough infection, T cells might produce one or two types of cytokines, Grifoni explains.
"After the breakthrough infection, the same cells produce multiple types of cytokines, making them more efficacious," says Grifoni. "Not only are our T cells not exhausted, but they are actually improving their capabilities."
The "immunity wall" does seem to have limits. Following an asymptomatic breakthrough infection, T cell abilities appeared to plateau in response to a subsequent symptomatic infection. B cells continued to produce neutralizing antibodies following subsequent breakthrough infections, but the researchers didn't see the same big "boost" to neutralizing antibody levels.
So should people continue to get SARS-CoV-2 booster vaccines? The LJI scientists point out that SARS-CoV-2 continues to evolve, and COVID-19 can still cause serious illness in immunocompromised people. Their advice is to follow all current CDC guidelines on who should receive booster vaccines.
Discovery may guide vaccine efforts
This research is also an important step toward the development of new vaccines against future SARS-CoV-2 variants and many other viruses with pandemic potential.Ramezani-Rad says the study helps answer important questions about how breakthrough infections alter antibody responses. Going forward, he is curious how future SARS-CoV-2 variants—or new vaccine designs—might further tweak the immune system.
"Studies of local B cell responses in the upper airway—where the infection occurs—will also be informative on how B cells responses are induced, particularly after breakthrough infection," says Ramezani-Rad.
Sette and Grifoni are focused on how to train T cells to recognize many types of coronaviruses at once. Their research is critical for developing a "pan-coronavirus" vaccine.
In a 2023 study, their laboratories worked with scientists at the University of Genoa to show that some T cells can recognize multiple coronaviruses at once. This new study shows them how breakthrough infections can shape T cell responses to fight novel SARS-CoV-2 variants.
"We're very interested to see if this phenomenon could be exploited in general to prepare against other potential pandemic threats," says Sette. "This is a step in a journey to help us protect against viral infections and potential pandemics."
Additional authors of the study, "SARS-CoV-2 breakthrough infections enhance T cell response magnitude, breadth, and epitope repertoire," include Tertuliano Alves Pereira Neto, Yeji Lee, Vanessa Silva-Moraes, Benjamin Goodwin, Nathaniel Bloom, Leila Siddiqui, Liliana Avalos, April Frazier, Zeli Zhang, Ricardo da Silva Antunes, and Jennifer Dan.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #836
Covid will still be here this summer. Will anyone care?
Despite “FLiRT” variants, this may be the first covid wave with little federal pressure to limit transmission or data to even declare a surge.By Fenit Nirappil
and
Sabrina Malhi
May 26, 2024 at 8:00 a.m. EDT
A person wearing a mask works the information desk of the Natural History Museum in D.C. on May 25. (Rosem Morton for The Washington Post)
Listen
8 min
Share
Comment4654
Add to your saved stories
Save
By now, it’s as familiar as sunscreen hitting the shelves: Americans are headed into another summer with new coronavirus variants and a likely uptick in cases.
This is shaping up to be the first covid wave with barely any federal pressure to limit transmission and little data to even declare a surge. People are no longer advised to isolate for five days after testing positive. Free tests are hard to come by. Soon, uninsured people will no longer be able to get coronavirus vaccines free.
“If a wave materializes this summer, we’re less poised to navigate the rough waters,” said Ziyad Al-Aly, an epidemiologist and long-covid researcher at the Veterans Affairs health-care system in St. Louis.
So we’re left with a virus that continues to hum in the background as an ever-present pathogen and sporadic killer. The public health establishment no longer treats covid as a top priority. Only a smattering of passengers still wear masks on trains and planes. Weddings, vacations and conferences carry on as normal. Many who do get sick won’t ever know it’s covid. Or care.
Covid returned to the headlines following the rise of new variants dubbed “FLiRT,” far catchier than the JN.1 variant that drove the winter wave. Leading the pack of those variants in the United States is KP.2, accounting for 28 percent of all infections as of early May, according to the Centers for Disease Control and Prevention. But public interest seems driven more by the name than the biological features of the variants, which appear unremarkable beyond the expected evolution of a virus to infect people more easily.
Follow Health & wellness
Follow
Summer offers a reminder of why covid is unlike the flu, a more predictable fall and winter respiratory virus. Coronavirus ebbs and flows throughout the year, and hospitalizations have always risen in summer months when people travel more and hot weather drives people indoors. For now, covid activity is low nationally, the CDC said Friday. The number of Americans dying of covid is less than half what it was a year ago, with a death toll around 2,000 in April. The virus poses a graver threat to the severely immunocompromised and elderly. But it can still surprise younger healthy people, for whom a bout of covid can range from negligible sniffles to rarer long-term debilitating effects.
What you need to know about covid this summer
1:28
People are no longer advised to isolate for five days after testing positive. Here are the CDC’s new guidelines for covid this summer. (Video: Drea Cornejo/The Washington Post)
When Lauren Smith, a 46-year-old triathlete in New Jersey, got covid in late April, she figured it would be a “nothingburger” like her first case two summers ago. Instead, she said she developed persistent fatigue for weeks that has made it difficult to train, and she decided to pull out of her upcoming competition. Her case is one that doctors would call mild, but Smith says doing so obscures the reality of a virus more complicated than the flu.
“There’s no care or attention given to the fact that this is serious,” said Smith, noting that she was one of the only masked attendees at a recent Guster concert in Philadelphia. “I feel like so many people have said, ‘I’m tired of this, I don’t want to deal with this anymore.’ And I don’t feel like the CDC or any other agency is doing anything to combat that.”
The Biden administration and the CDC don’t talk much about covid anymore, save for sporadic updates on data and variant tracking, and the president’s criticism, when campaigning, of his predecessor’s handling of covid. CDC Director Mandy Cohen hasn’t tweeted about covid since March. The agency declined to make an official available for an interview about its response.
The CDC and health authorities continue to promote the coronavirus vaccine, last updated in fall 2023 for a subvariant no longer in circulation, as the best form of protection against the disease. Just 23 percent of adults have received a dose of the latest vaccine, the CDC estimates. Experts say the existing formula should still confer protection against severe illness from the FLiRT variants. People 65 and older qualify for a second dose, but only 7 percent have received two shots.
Masks and gloves at a Wegmans grocery store. (Rosem Morton for The Washington Post)
Expert advisers to the Food and Drug Administration are scheduled in June to recommend the composition of the coronavirus vaccine to be released in the fall to protect against the latest variants.
But people without health insurance will no longer qualify for free vaccines under the CDC’s Bridge Access Program, which ends in August after providing more than 1.4 million free shots. Funding for the program ran out, and efforts to establish a broader national program offering free vaccines for adults have languished.
Peter Hotez, co-director of the Texas Children’s Hospital Center for Vaccine Development, said declining covid data collection will make it harder to persuade Americans that the virus poses enough of a threat to merit getting vaccinated.
In April, hospitals stopped reporting confirmed covid-19 cases — ending the most commonly cited metric for measuring the virus’s toll. The CDC still tracks the levels of coronavirus detected in wastewater and discloses the percentage of emergency room visits with a diagnosed covid-19 case, which has been declining since February. But Hotez said the available metrics are no longer enough to properly grasp the covid situation.
“We’re kind of shooting blind now,” said Hotez, who is also dean of the National School of Tropical Medicine at Baylor College of Medicine.
Public health officials treat covid with less urgency in part because hospitals no longer report that covid patients pose a significant threat to their capacity.
Raynard Washington, who leads the Mecklenburg County health department in North Carolina, noted that while covid remains deadlier and more transmissible than the flu, the virus has become far more manageable because of vaccination.
“It’s not causing disruption to our everyday life like it used to,” Washington said.
While health-care systems can manage covid waves, Otto Yang, associate chief of infectious diseases at UCLA’s David Geffen School of Medicine, said the immunocompromised and older adults at high risk of developing severe disease are often overlooked.
A masked person in a crowd of travelers at Reagan National Airport on May 25. (Rosem Morton for The Washington Post)
“Those people unfortunately carry a heavy burden,” Yang said. “I’m not sure there is a good solution for them, but one thing could be better preventive measures.”
The covid protection measures that were a staple of earlier summers — requests to test before attending weddings, mask requirements at conferences, outdoor locations for celebrations — are falling by the wayside.
Many summer campers, for instance, will no longer be forced to isolate for covid while asymptomatic since the CDC revised its quarantine protocols to allow people to reemerge after their fevers break, said Tom Rosenberg, president and chief executive of the American Camp Association. But other covid protections have stuck: Opening windows to improve ventilation, screening for symptoms of illness and discouraging parents from helping their kids unpack when they arrive. Regardless of the pandemic’s severity, Rosenberg said, camps seek to minimize disruptions from illness.
“Kids can have more fun,” Rosenberg said. “We want to keep them in camp as much as we can as long as they are well and ready to participate.”
Others trying to keep precautions in place face greater challenges as they become outliers.
Organizers of Dyke Fest, an LGBTQ+ community gathering in D.C., wanted to be inclusive of immunocompromised people when they asked attendees to wear masks and test before coming to a bar where more than 250 attendees drank, browsed jewelry and art, and joined packed crowds watching drag performances. But compliance was spotty and enforcement tricky when rain drove people indoors, where drinking and masking don’t easily mix, and pandemic masking norms have eroded.
“Culturally we are coming away from it as a society, so it gets much harder to ask people to really be consistent, because they aren’t doing it anywhere else,” said D Schwartz, one of the organizers. “You go into a movie theater now, you see maybe five people wearing a mask.”
Medically vulnerable people are adjusting to a world where they can’t count on people to mask anymore, even at the doctor’s office. In North Carolina, Republican lawmakers proposed legislation in May that would criminalize mask-wearing in public, even for medical reasons, in response to growing protests against the war in Gaza, where many protesters have worn medical masks.
Masks are no longer common on public transit in D.C. (Rosem Morton for The Washington Post)
The proposal floored Cat Williams, who received a double lung transplant and faces heightened danger from covid infections because she takes medication that suppresses her immune system. At medical appointments, she has had to plead with medical staff to cover their faces while she gets her blood drawn and undergoes X-rays. The prospect of getting arrested for wearing a mask and being forced to take it off in a crowded jail makes her even more fearful to leave home. And she worries mask skeptics will be emboldened to harass people who wear them.
“We have a target on our backs,” said Williams, 53, of Charlotte. “They don’t want anyone to give them the reminder that covid is around.”
Clara Ence Morse contributed to this report.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #837

mpox and COVID-19 vaccines can be safely given at the same time, says advisory body
The National Advisory Committee on Immunization says the mpox vaccine can be given at the same time as an mRNA COVID-19 vaccine, reversing its previous recommendation to wait at least four weeks due to safety concerns.
mpox and COVID-19 vaccines can be safely given at the same time, says advisory body

The Canadian Press
Staff
Contact
Updated May 24, 2024 6:59 p.m. EDT
Published May 24, 2024 3:31 p.m. EDT
Share
- Link
- X
It said Friday that data is now available to show there is no increased risk of myocarditis or anaphylaxis for people who are given Imvamune, the vaccine for mpox, when they are also vaccinated against COVID-19.
The recommendation also says that Imvamune can be given at the same time as any other live or non-live vaccines.
The committee recommended the mpox vaccine two years ago after outbreaks in several countries, mostly among men who have sex with men as well as sex workers.
RELATED STORIES
- 'A really bad car crash': Why health experts are raising concerns over surging syphilis cases
- Discrimination is killing queer people, says LGBTQ2S+ advocacy group
- Toronto holding mpox vaccine clinics as cases of the virus spike
- The information you need to know, sent directly to you: Download the CTV News App
Ontario had 737 cases, Quebec reported 531 cases and British Columbia had 213, the committee said.
Symptoms of the disease include a rash, fever, body aches, back pain and swollen lymph glands that appear within seven to 21 days after exposure.
Two doses of Imvamune are given at least 28 days apart to protect against the disease or as soon as possible after exposure to the virus to prevent illness or severe outcomes.
Those considered at highest risk of mpox include men who have sex with men and meet at least one of these criteria: they have more than one partner, are in a relationship where at least one of the partners has other sexual partners or they have had a confirmed sexually transmitted infection in the last year.
The committee says sex workers, regardless of gender or sexual orientation, are also at risk of infection, as are people who have had sexual contact in sex venues or work or volunteer there.
It says that while cases of mpox have declined significantly since the fall of 2022, the disease remains an important public health concern.
A spokeswoman with Toronto Public Health says the city has had 36 lab-confirmed cases so far this year compared to 27 cases for all of last year.
Toronto Public Health says the mpox vaccine will be offered by appointment at Metro Hall on June 1 and June 8 as part of Pride month awareness efforts that will also involve community organizations.
This report by The Canadian Press was first published May 24, 2024.
Canadian Press health coverage receives support through a partnership with the Canadian Medical Association. CP is solely responsible for this content.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #838

Covid pandemic cut global life expectancy by nearly two years: WHO
Covid-19 cut global life expectancy by almost two years when it raged from 2019 to 2021, wiping out a decade of progress, the World Health Organization said Friday.
MAY 24, 2024
Editors' notes
Covid pandemic cut global life expectancy by nearly two years: WHO

Covid-19 cut global life expectancy by almost two years when it raged from 2019 to 2021, wiping out a decade of progress, the World Health Organization said Friday.
"The Covid-19 pandemic reversed the trend of steady gain in life expectancy at birth and healthy life expectancy at birth," the UN health agency said.
Global life expectancy fell 1.8 years to 71.4 years, the same level as it was in 2012, according to a WHO annual world health statistics study.
The amount of time the average person can expect to live in good health fell 1.5 years to 61.9 years in 2021 -- also the 2012 level, the study said.
The impact was even worse than the findings of a study published by the Lancet in January, which said average life expectancy fell 1.6 years during the pandemic.
Researchers for that study said Covid-19 had a "more profound impact" on life expectancy than any other event over the past half century.
WHO director general Tedros Adhanom Ghebreyesus said the figures highlighted the importance of the global pandemic security accord being negotiated in Geneva "to strengthen global health security, but to protect long-term investments in health and promote equity within and between countries".
The Lancet researchers estimated that Covid-19 caused 15.9 million excess deaths during 2020-2021, either from the virus or pandemic-related disruption to health systems.
The WHO study said however that life expectancy did not fall in the same way around the world.
The Americas and Southeast Asia were the worst-hit regions, with life expectancy falling by about three years, it said.
The Western Pacific was the least hit, with life expectancy falling just 0.1 year.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #839

Covid-19 update: 6636 new cases and 7 further deaths
There have been 6636 new cases of Covid-19 reported in the past week, and seven further deaths attributed to the virus.
Covid-19 update: 6636 new cases and 7 further deaths
3:31 pm on 27 May 2024Share this
- Share on Twitter
- Share on Facebook
- Share via email
- Share on Reddit
- Share on Linked In

Photo: 123rf.com - RNZ / Composite Image - RNZ
There have been 6636 new cases of Covid-19 reported in the past week, and seven further deaths attributed to the virus.
It comes as epidemiologist professor Michael Baker says New Zealand is at its highest peak for the virus in 18 months.
There were 282 cases in hospital as of midnight on Sunday, the Ministry of Health said.
The seven-day rolling average of cases was 948. Of the total new cases in the past week, 4338 were reinfections.
Epidemiologist professor Michael Baker on Monday told RNZ's First Up one in three people were still contagious five days after testing positive.
As winter approaches, so too does Covid-19 duration7′ :52″
from First Up
Add to playlist
Download
- Download as Ogg
- Download as MP3
- Download as AAC
- Play Ogg in browser
- Play MP3 in browser
- Play AAC in browser
Despite the recommended isolation period now only being five days, Baker suggested people still getting a positive Covid-19 test wait to test again on day 6 or 7 before going back into society.
Last week, the ministry reported 6146 new cases of the virus and 19 further deaths.
"The biology hasn't changed," Baker said, but there was more pressure for people to go back to work and school.
Baker said he would like to see money in this week's Budget going towards the Covid-19 response.
It was important for health and productivity that the government continued to fund booster shots, RAT tests and the anti-viral medication.
As soon as people had to pay for these, low income households would miss out.
Baker said it had to remain fair and equity had to be maintained.
Last week, the ministry reported 6146 new cases of the virus and 19 further deaths.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,194
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #840
Respiratory Virus Report, Week 20 - ending May 18, 2024 - Canada.ca
Respiratory Virus Detection Surveillance System data from Canadian laboratories on the number of tests, and positive tests, for influenza and other respiratory viruses.
Respiratory Virus Report, Week 20 - ending May 18, 2024
Organization: Public Health Agency of Canada
Please note that the Respiratory Virus Detection Surveillance System (RVDSS) is a sentinel laboratory surveillance system that does not capture all respiratory virus testing performed in Canada; differences may exist between the data presented in this report and provincial/territorial epidemiological reports. SARS-CoV-2 laboratory data is included in this report to facilitate the comparison of positivity with other respiratory viruses. Interpretation should be made with caution as testing practices differ among viruses.
For additional SARS-CoV-2 surveillance information, please refer to the COVID-19 epidemiology update.
Overall summary
In week 20 (week ending May 18, 2024) in Canada, percent positivity is currently highest for enterovirus/rhinovirus (10.5% positive) among respiratory viruses under surveillance. The following results were reported from RVDSS laboratories:- After reaching a low in early-April 2024 (4.7% positive), national SARS-CoV-2 percent positivity continues to increase (2,048 detections; 8.2% positive). Trends currently vary by region.
- Influenza percent positivity continues to decrease (723 detections; 3.1% positive) and is now below the epidemic threshold. The end of the influenza season at the national level occurred in week 19 (week ending May 11, 2024).
- RSV percent positivity is stable (212 detections; 1.0% positive).
- Percent positivity of all other non-SARS-CoV-2 respiratory viruses is near expected levels typical of this time of year.
- 34/35 sentinel laboratories reported surveillance data
Users who are viewing this thread
Total: 1 (members: 0, guests: 1)
Pakistan Defence Latest
-
-
-
The Dark Legacy of Former DG ISI Nadeem Anjum: A Tale of Constitutional Breaches and Human Rights Violations (2 Viewers)
- Latest: lightning f57
-
Country Watch Latest
-
Not just engines, Tejas Mk-1A delivery could be hit over key Danish part, now on export blacklist (8 Viewers)
- Latest: Yasser76
-
-
-
Latest Posts
-
SC rebukes ‘misconceived’ ECP clarification request, orders immediate implentation of reserved seats verdict (5 Viewers)
- Latest: M. Sarmad
-
-
Not just engines, Tejas Mk-1A delivery could be hit over key Danish part, now on export blacklist (8 Viewers)
- Latest: Yasser76
-
'Indus Water Treaty Not feasible to maintain': India serves notice to Pakistan, seeks Modification. (6 Viewers)
- Latest: Ali_Baba
