Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,628

Summer COVID wave as high as winter, bucking the normal pattern
This summer has seen a steady increase in COVID cases, in contrast to a previous, gradual decline in summer cases since the pandemic.
Summer COVID wave as high as winter, bucking the normal pattern

Dr. Mark Jaben
This summer has seen a steady increase in COVID cases, in contrast to a previous, gradual decline in summer cases since the pandemic.
“Each summer has seen a smaller wave than corresponding winter. And each summer wave has been smaller than the previous summer,” said Dr. Mark Jaben, Haywood County medical director, in a recent Covid update video. “Not so this summer — more cases now than last summer, and for Haywood County, as many cases now as this past winter.”
Hospitalizations now are as high as during the winter surge in February. The good news is, the hospitals are not seeing an increase in deaths that might be anticipated.
But what is causing the summer rise? Jaben attributes it to three factors:
Weather: Hot summer temps keep more folks indoors. The virus spreads more readily in enclosed places.
Vaccinations wearing off: The immune wall that exists with prior infections and vaccinations wears off over time. Less than 20% of the population is up to date with vaccination.
Mutations: The virus continues to mutate, and the latest variants are more capable of evading our defenses.
It’s important that folks are attentive to the spikes in Covid to prevent the spread of disease to those who are immunocompromised or elderly, Jaben said.
Jaben also recommends updating your vaccination if it’s been six months since your last one. It will still protect you from more severe symptoms, but full prevention has likely worn off. Last fall’s updated vaccine remains effective based on the JN.1 variant that accounted for nearly 100% of infections this past winter, he said.
Jaben predicts the new vaccine will be available in September, and effective against the variants we see now, like KN and LB. But should you get vaccinated right now or wait for the new one? Jaben said it can be tricky to gauge. If you got vaccinated last fall, winter or spring, it might make more sense to wait on the upcoming vaccine.
Free COVID tests are available in the Haywood County Health Department lobby.
If you do have COVID, isolate until symptoms improve and there’s no fever for 24 hours while you’re off fever-reducing medicine, Jaben said. Then wear a mask around others for an additional five days.
Last edited:
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,629
Log in to Facebook
Log in to Facebook to start sharing and connecting with your friends, family and people you know.
 www.facebook.com
www.facebook.com
Janet Hanlin
AdminTop contributor
· oeSndpstro4141hafiu37h61gaa4hh8cmh8mg8a15lm401lm92371lh0g2lt ·
Weekly Ontario Update for Friday, August 2, 2024:
Public Health Ontario has published their last wastewater report. Unless indicated otherwise, information in this update includes data from Sunday, July 21 to Saturday, July 27, so data is delayed.Data relating to deaths is even further delayed as cause of death is taking MONTHS to be determined. So recent deaths will end up being far WORSE in the future than are being reported for today.
- Recent cases: This number is no longer being reported!
- Weekly positivity rate: 12.2% (+ 0.9% since last week)
- Recent deaths: 3 (- 5) Recent deaths are a lagging indicator of the current level of new cases. Deaths are underreported because they are based on date of death and by the time the cause of death is reported, it is no longer considered recent!
- Average daily hospital bed occupancy: 427* (- 9 since last week week) *Please interpret the COVID-19 hospitalization data with caution as not all centers are reporting..
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,630
An update on COVID in Manitoba
Dr. Brent Roussin discusses Manitoba’s COVID-19 numbers, the latest strain and wastewater testing results
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,631

Fired health-care workers can reapply for their jobs, but some don't want to
A former Island Health laundry worker who declined to be vaccinated for COVID-19 says he’s making more money in construction.
 www.timescolonist.com
www.timescolonist.com
Fired health-care workers can reapply for their jobs, but some don't want to
A former Island Health laundry worker who declined to be vaccinated for COVID-19 says he’s making more money in construction.
Cindy E. Harnett
about 5 hours ago

An Island Health worker who lost his job after refusing to be vaccinated for COVID-19 says he might return to work in a casual position if his employer would hire him back, now that vaccine mandates have ended.
Then again, Jedediah Ferguson, who worked in the laundry department of Cumberland Regional Hospital, says he’s making more money in construction. “[The mandates] should have been rescinded a long time ago. B.C. is pretty much the only place on the planet that has those mandates in place.”
Ferguson, who was among almost 2,700 health-care workers fired over the mandate, is one of the petitioners in a class-action lawsuit that seeks compensation on behalf of all unionized health-care workers subject to the vaccine mandate.
The COVID-19 public health emergency declared March 17, 2020 — which included mask mandates, vaccination requirements, and restrictions on gathering and long-term care visits — ended on July 25. The vaccine mandate that was introduced October 2021 and renewed each of the two following years ended also.
Fired workers can reapply for their jobs but anyone working in public health-care facilities, including volunteers and contract workers, will be required to report their immunization status for COVID-19 and other communicable vaccine-preventable diseases, including mumps and measles.
The measure is intended to guide staffing decisions — from masking to re-assigned duties to temporary exclusion from work — in the event of future outbreaks or pandemics.
The B.C. Nurses Union says it will monitor any impact of the registry to ensure workers’ rights are protected.
Ferguson said he didn’t get vaccinated for COVID-19 because he didn’t believe the vaccine was effective. Because he worked in the laundry, a non-clinical facility, he felt he didn’t pose a risk to vulnerable patients.
Another petitioner in the class-action lawsuit, Terri Perepolkin, who was a lab tech at Vernon Jubilee Hospital in Vernon, said Henry is two years late in dropping the vaccine mandate, but it’s a step in the right direction.
“But I mean, it’s not stopping us or our lawsuit, because we weren’t suing to get the mandates dropped. We’re not suing to get our jobs back,” she said. “We’re suing to get compensation for the mistreatment that that was put on us, right?”
Perepolkin, who currently has no plans to re-apply for her job, said she and her children are immunized against other diseases, but she isn’t sold on flu vaccines and didn’t believe the COVID vaccine had been sufficiently tested at the time it was offered.“I want vaccines to work. I want them to be great.”
Perepolkin argues there’s no difference now between vaccinated and unvaccinated health-care workers because almost everyone’s had the disease or the vaccine, and immunity from 2021 shots has waned. “So no, there’s absolutely zero risk when you compare an unvaccinated person to someone who had [the vaccine] years ago.”
Victoria lawyer Umar Sheikh of Sheikh Law, which is leading the class-action suit, said in an email the government knew early on that the COVID vaccine was “ineffectual” at stopping the spread of the disease, yet continued to fire health-care workers for not getting it.
Sheikh maintains the government mandates have critically reduced health-care staffing that was already stretched. Those affected by the mandate should be offered their jobs back with back pay and full restitution, he said.
The Health Ministry said the 2,692 employees terminated as of July due to non-compliance with the provincial health officer’s vaccine order represent less than 1.2 per cent of those employed in B.C.’s public-health sector.
Of the fired workers, 484 — including 69 casual staff — are in the Island Health region. In emergency departments, one full-time, one part-time and five casual nurses were fired.
Health Minister Adrian Dix said after the vaccine mandate came into effect, B.C. led the country in the recruitment of nurses, doctors, health-sciences professionals and other health-care workers.
In 2022, B.C. had 38,935 nurses, up from 35,88 from 2020-2022, according to data from the Canadian Institute for Health Information. In Alberta, where there was no mandate, the number of health-care workers decreased, Dix said.
Dr. David Forrest Forrest, an infectious-disease specialist at Nanaimo Regional General Hospital, said he doesn’t expect the end of the vaccine mandate to have a meaningful impact on health-care worker staffing or availability.
As a health-care professional interacting, sometimes closely, with vulnerable patients, Forrest said he believes it’s his “ethical obligation” to undertake measures — from hand-washing to vaccination and masking — to reduce the risk of transmitting infectious pathogens to patients.
Forrest acknowledges that vaccination “only transiently” reduces the risk of acquiring and transmitting many, especially viral, diseases. But he said for those not following infection-control measures such as vaccination or mandatory masking, assignment to alternate duties is “not unreasonable.”
Aside from the effects on patient care, mandated vaccination can help help reduce health-care workers’ sick days by reducing the severity of infection, he said.
Dr. Réka Gustafson, Island Health chief medical health officer, called the risk that a health-care worker who is not vaccinated for COVID-19 poses for patients and colleagues “very negligible,” given that the vast majority of people who are vulnerable have been vaccinated.
She said that since COVID-19 has turned out to be “not strongly seasonal” and can repeatedly infect someone, the primary benefit of vaccination is now to the person being vaccinated.
In other communicable diseases, if the vaccine prevents you from getting infected for life, you can’t spread it to others.
Gustafson said it’s important to turn to other pressing health issues, such as the toxic-drug crisis, which killed 1,158 people in the first six months of this year, the BC Coroners Service recently reported.
Declared a public health emergency in 2016, the toxic-drug crisis has resulted in close to 15,000 deaths so far.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,632
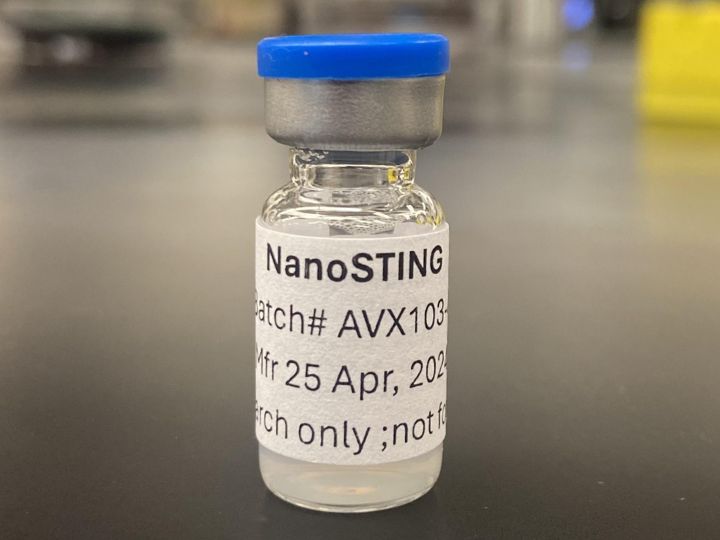
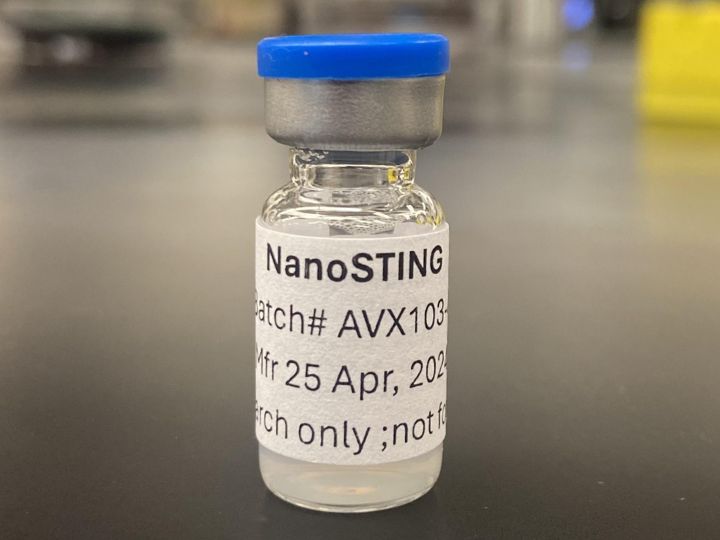
UH researchers have developed two nasal sprays for respiratory viruses, COVID-19 | Houston Public Media
Both sprays are developed to function by heightening the immune system in a person's nose.
UH researchers have developed two nasal sprays for respiratory viruses, COVID-19
Both sprays are developed to function by heightening the immune system in a person’s nose.Patricia Ortiz | Posted onAugust 7, 2024, 12:39 PM
Twitter/X
University of Houston
NanoSTING (and NanoSTING-SN) developed at UH to fight COVID and flu.
University of Houston researchers have developed two new nasal sprays for respiratory viruses like the flu and COVID-19.
Dr. Navin Varadarajan is an MD Anderson Professor at the University of Houston. He said one spray is a therapeutic, and the other could be a universal vaccine that prevents transmission for many COVID variants, which are airborne.
"The therapeutic will have a maximum impact on people who are immunocompromised to try and restore their immunity by activating it. Then, they're protected from hospitalization,” he said.
The therapeutic nasal spray would be taken when someone is already showing symptoms, Varadarajan said, like taking Tylenol for a headache.
The National Institute of Health has also sponsored a different nasal spray for COVID-19 in development and opened clinical trials last month. Some of the trials will take place at the Baylor College of Medicine in Houston.
Both UH sprays are developed to function by heightening the immune system in a person’s nose. Varadarajan said that separates these sprays from others in development.
“Our approach is somewhat different because we harness the immune system. We don’t exactly attack the virus,” he said. “Nothing in our formulation exactly attacks the virus, instead it activates your body’s immune system so that the immune system in your nose is in a heightened state of alert and is then able to tackle the virus.”
He said it could still take a while before their nasal sprays are commercially available, but clinical trials might start up in a year. Varadarajan said he found this project to be rewarding.
“We do science because we want to be able to make a difference to people in human lives, and to having the opportunity to be able to work on something that can make it to humans and hopefully have the same effect in humans, is very rewarding,” he said.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,633

COVID behind death of seven New Brunswickers in July
Province saw 253 cases confirmed last month, according to Health Department data
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,634

COVID still 'very much with us' amid summertime surge, WHO warns
The World Health Organization (WHO) is urging governments to strengthen vaccine campaigns.
COVID still 'very much with us' with 20% of tests positive in Europe, WHO warns

Copyright AP Photo/Nam Y. Huh
By Euronews
Published on 07/08/2024 - 11:49 GMT+2•Updated 14:24
The World Health Organization (WHO) is urging governments to strengthen vaccine campaigns.
COVID-19 is "still very much with us," World Health Organization (WHO) officials warned this week, adding that cases are rising globally, with a high percentage of positive tests in Europe.
“Data from our sentinel-based surveillance system across 84 countries reports that the per cent of positive tests for SARS-CoV-2 has been rising over several weeks,” said Dr Maria Van Kerkhove, the COVID-19 technical lead at WHO.
"Overall, test positivity is above 10 per cent, but this fluctuates per region. In Europe, per cent positivity is above 20 per cent," she added.
At least 40 athletes at the Olympic Games have tested positive for COVID-19 or other respiratory illnesses, the WHO added in a statement on Wednesday.
Many countries have also experienced surges of the virus regardless of the season and the circulation of the virus is likely much higher than reported.
Dr Kerkhove said that governments should "continue to invest and support our global understanding of the circulation and impact of this virus and to provide their populations with the tools to protect themselves".
She also urged individuals to protect themselves by getting vaccinated.
"Over the last two years, we have seen an alarming decline in vaccination coverage, especially among health workers and people over 60, two of the most at-risk groups," she said.
"This urgently needs to be turned around".
This article has been updated with a new statement from WHO on the number of athletes with respiratory viruses at the Olympics.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,635

Amid a COVID summer spike, why are so few Floridians getting the vaccine?
Health experts say the public's relationship with the virus has changed. And that’s leaving them concerned.
health.wusf.usf.edu
Amid a COVID summer spike, why are so few Floridians getting the vaccine?
Central Florida Public Media | By Joe Mario PedersenPublished August 7, 2024 at 7:52 AM EDT
Listen • 1:43

Lisa Ferdinando
/
Department of Defense, file
In 2021, the first full year a COVID-19 vaccine was available, 15 million Floridians received a vaccine. But this year, a little over 400,000 have received a booster, despite the virus's summer spike.
Health experts say the public's relationship with the virus has changed. And that’s leaving them concerned.
As the number of COVID-19 cases rises in Florida, vaccination rates lag behind, and that is concerning health experts.In 2021, the first full year a COVID-19 vaccine was available, 15 million Floridians received a vaccine. But this year, a little over 400,000 have received a booster, despite the virus's summer spike.
“I think that people at this point have a little bit less concern about getting infected with COVID,” said Cindy Prins, an epidemiologist at the University of Central Florida. “I don't think they’re necessarily correct.”
Hospitalizations and emergency department visits are increasing throughout the country, according to the Centers for Disease Control and Prevention.
The numbers and the severity
Meanwhile, in Florida, monthly case totals increased to 94,000 in July – the highest of the year, according to the state Department of Health. June reported a total of 38,000 cases.
The majority of cases reported are the highly transmissible omicron subvariant strains.
While the virus spreads quickly, it doesn’t pack the same punch that it used to for most people, said Jerne Shapiro a professor of epidemiology at the University of Florida.
“The virus no longer infects the lower part of our lungs and upper part of our respiratory system, which has really decreased the number of individuals that die from COVID and the number of individuals that require hospitalization,” she said.
With a higher infection but lower severity comes a less-perceived risk for the general population, which is one the reasons vaccine levels are probably low, Shapiro said.
“However, there is still a portion of the population that is at an increased risk for severe outcomes,” including those with autoimmune deficiencies or 65 and older, Shapiro said. “That is where we really want to make sure those individuals understand that they're at risk and understand how to access the vaccine.”
Why are vaccine rates lower?
Vaccine rates have been dropping since their 2021 peak in Florida. A number of factors are responsible, like COVID news fatigue and people not keeping up to date with vaccines, Prins said.
She thinks time has also warped people’s memories of what it’s like to have COVID.
“I think that's another thing that we tend to forget, that it can be a really miserable disease, and even if you didn't have a bad bout of it last time if you get it this time, you may have a lot more problems with it, and you may feel quite miserable,” Prins said.
The rising rate of COVID and the low rate of vaccines represent a larger threat to those in a risk group.
Why it's a problem
What concerns Shapiro is the combination of high case rates and low vaccine levels as schools get ready to bring students back into the classroom. Most children are not at risk for severe infection, but they may have family members who are. Additionally, more COVID cases could strain the medical system, she said.
“We are testing. We're seeing those increases, and we are also seeing an increase in our emergency department visits,” Shapiro said. “We can expect, as our early indicators show, increased positivity, increased COVID rates, that our hospitalization and deaths will continue to increase over the next few weeks, maybe even a month or two.”
Epidemiologists don’t have a lot of historical data for COVID, but the past two years have shown summer spikes followed by a drop in cases before Thanksgiving. Prins is hopeful that this will happen again.
Although, she’s still concerned.
If trends hold, and COVID vaccines continue to become less popular while the virus is allowed to mutate and keep infecting, she’s not sure what kind of future that presents Florida and its medical system.
“If you have more transmissible and more variants that are a little bit scarier in terms of health outcomes, and people have this mindset of 'I don't need the vaccine.' I think that's where we potentially run into a problem and a concern if people are not wanting to get vaccinated,” she said.
Current guidelines
The CDC advises that everyone age 6 months to 64 years should receive one vaccine a year. Those 65 and older and those with immune deficiencies should receive it twice a year.
The Florida Department of Health advises only those over 65 or in a risk group to get the vaccine.
The vaccine is available at most pharmacies and grocery stores. A new vaccine is expected to come out in the fall to protect against winter strains.
Copyright 2024 Central Florida Public Media
Users who are viewing this thread
Total: 4 (members: 0, guests: 4)
Pakistan Defence Latest
-
Israel and USA 'jammed GPS signals' in days before Iran's 300-missile launch to confuse attackers (21 Viewers)
- Latest: Cash gk
-
-
A GIDS Shahpar II UAV of the PAF broke midair and crashed near Darya Khan, Punjab (3 Viewers)
- Latest: Broghil
-
-
Country Watch Latest
-
Pakistan to Deliver First Batch of Anti-Tank Guided Missiles to Bangladesh (12 Viewers)
- Latest: Asfandyar Bhittani
-
Why India Deliberately kept Weakened Bangladesh’s Military | InShort (7 Viewers)
- Latest: Vikramaditya1
-
Not just engines, Tejas Mk-1A delivery could be hit over key Danish part, now on export blacklist (5 Viewers)
- Latest: Circadian Rhythm
-
-
Latest Posts
-
Israel and USA 'jammed GPS signals' in days before Iran's 300-missile launch to confuse attackers (21 Viewers)
- Latest: Cash gk
-
SC reserved seats ruling can't be implemented after amendments to Election Act: NA speaker (4 Viewers)
- Latest: prothought
-
-
