Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,636

COVID-Positive Olympic Athletes Are Still Competing
Several athletes at the Paris 2024 Olympic Games have come down with COVID, but they are still allowed to compete
August 7, 2024
3 min read
COVID-Positive Olympic Athletes Are Still Competing
Several athletes at the Paris 2024 Olympic Games have come down with COVID, but they are still allowed to competeBy Saima S. Iqbal

Adam Peaty of Team Great Britain competes in the Men’s 100m Breaststroke Final on July 28 at the Olympic Games Paris 2024 in Nanterre, France. Peaty is among several athletes who have tested positive for COVID.
Around 11,000 of the world’s top athletes have gathered in Paris to compete in the 2024 Summer Olympics. In the past two weeks, at least 19 have tested positive for COVID. Many of these athletes compete for Australia or are in aquatic sports. The current count includes, for instance, British swimmer Adam Peaty and Australian swimmers Lani Pallister and Zac Stubblety-Cook. Although only a small fraction of the competitors are known to be infectious, some experts fear a wider outbreak; in the absence of testing requirements, it’s possible many more participants could harbor the COVID-causing virus SARS-CoV-2.
The Tokyo 2020 Summer Olympics and Beijing 2022 Winter Olympics implemented strict rules to limit the spread of COVID, including regular testing, social distancing and near-constant mask wearing. The Paris 2024 Olympic Games, by contrast, aim at a return to normalcy. It’s not just that thousands of spectators now fill the stands, where they were once banned. The Paris Games also drop all previous COVID protocols, instead approaching the disease like other respiratory illnesses such as the common cold or the flu: officials now allow athletes and teams to determine for themselves how to prevent or respond to infection.
Athletes no longer undergo daily testing or frequent temperature checks. Players who feel ill are encouraged—though not required—to wear masks, wash their hands and avoid close contact with others. The Olympic Village has single rooms available for athletes who test positive for COVID, and certain countries, such as the U.S., provide separate transportation for sick participants. Infected athletes may still train and compete in events—and so far many have. A handful have dropped out of certain events to save their energy for others, and one athlete, German decathlete Manuel Eitel, has left the games altogether.
SARS-CoV-2 still has the potential to disrupt the remaining events, especially if entire teams catch it. “It makes sense to be more aware of [the virus] moving forward,” says Peter Chin-Hong, an infectious disease doctor at UCSF Health. “We still have a ways to go in the Olympics.”
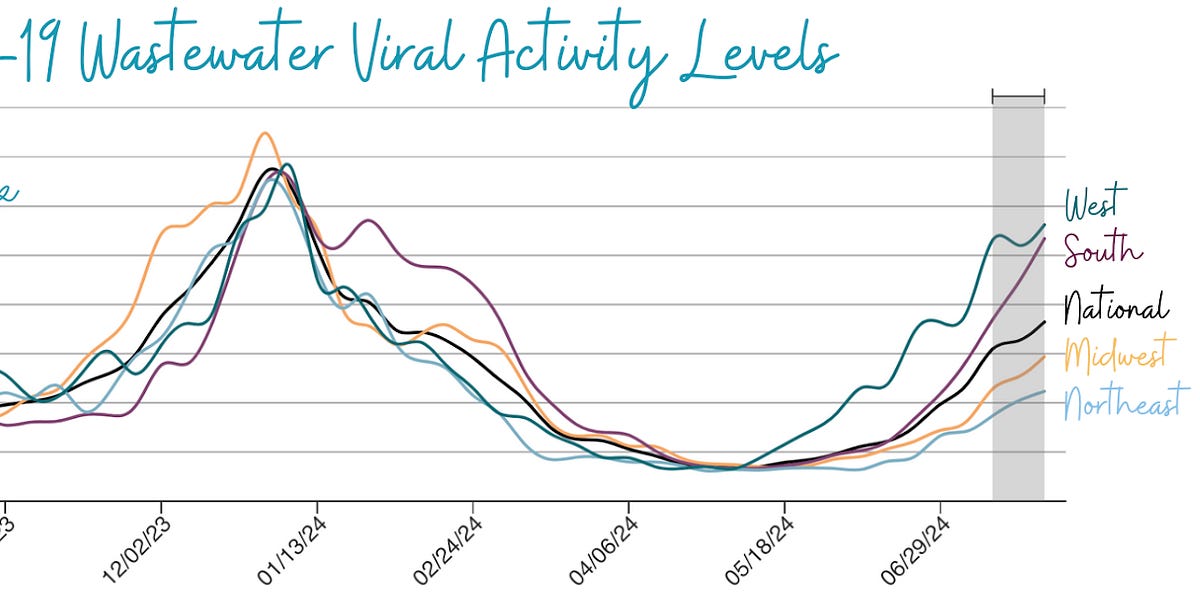
As a large, congregate setting full of panting and shouting people, the Olympic Village provides “picture-perfect ways to spread” respiratory illness, Chin-Hong notes. But unlike the flu or the common cold, COVID is now surging across the U.S. and many regions of Europe, thanks in part to new, more transmissible strains of SARS-CoV-2. Athletes who compete in contact sports or in sites with poor ventilation may be at the highest risk for infection, but all athletes frequent danger zones such as the locker room or the dining hall.
COVID also takes a more serious toll on the body than either colds or the flu, Chin-Hong says. While most Olympic athletes are healthy and have access to cutting-edge medications, young people sometimes display mixed responses to infection. Athletes with comorbidities, such as U.S. gymnast Sunisa Lee, who lives with kidney disease, or U.S. swimmer Katie Ledecky, who has postural orthostatic tachycardia syndrome, may be more vulnerable than others. And even mild COVID symptoms can impair a person’s performance.
One 2024 study of several hundred German athletes found that elite athletes infected with COVID had milder infections than nonelite ones. But more than half of these elite athletes said their symptoms—which included headaches, cough, fever and sore throat—hampered their training for two to four weeks. And several months later 10 percent of them reported trouble concentrating and a drop in their performance. A 2023 survey of more than 800 elite aquatic athletes showed that 16 percent of those infected had no symptoms; 51 percent had mild symptoms; and 27 percent had moderate ones, with 10 percent of athletes developing long-term symptoms such as fatigue and shortness of breath.
Infectious competitors can also sicken coaches and staff, who tend to be older and therefore at greater risk for serious illness. Several team members with sick athletes are now wearing masks, the Guardian reported.
Officials from the Paris Games told Scientific American that they are working closely with France’s Ministry of Health to monitor further spread of SARS-CoV-2. The week the games began, French health minister Frédérick Valletoux reassured the public that he had little reason to fear an outbreak. COVID cases in the country have risen over the summer, but they remain at “a low rumble,” he said in a July 25 broadcast interview.
On August 6 a representative of the World Health Organization stressed in a United Nations press briefing that rates of COVID have increased all over the globe in the past few weeks, demanding further vigilance. In Europe more than 20 percent of COVID tests have been positive in recent weeks.