Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,652

COVID Summer Surge: How to Get Free Tests to Keep Yourself Safe and Informed
Contagious new COVID-19 variants have led to a rising number of infections this summer.
COVID Summer Surge: How to Get Free Tests to Keep Yourself Safe and Informed
Contagious new COVID-19 variants have led to a rising number of infections this summer.Mary-Elisabeth Combs,
Peter Butler,
Katie Teague
Aug. 5, 2024 7:45 a.m. PT
5 min read

The USPS stopped shipping free COVID-19 tests back in March.
Stephen Shankland/CNET
It seems like nothing is safe from COVID-19 this summer -- the Paris Olympics and San Diego's Comic-Con have both shown how quickly COVID is spreading. Whether it's the heat waves or the new COVID variants that are to blame, doctors are saying that this summer is much worse than the last.
California was one of the first states this summer to report rising COVID cases, but it's not the only one -- 21 states and Washington DC are all displaying "high levels" of COVID-19 in their wastewater, per the CDC. If you're planning on spending time indoors with other people, especially for extended periods of time, at-home COVID-19 tests can be essential for keeping your loved ones safe.
Read more: Are Your COVID Tests Really Expired? How to Find Out
Back on March 8, 2024, the Federal Government halted the US Postal Service's free COVID program, which would allow you to order free COVID-19 tests through the USPS. However, hope is not lost when it comes to getting free tests to detect COVID-19 infections. Read on to find out the ways you can still get free COVID testing, as well as how to get your hands on free treatments and COVID vaccines.
For more, here's what to know about long COVID, and all of the latest information about bird flu in humans.
What are my free COVID-19 testing options?
Now that you can no longer receive tests from the Postal Service, you have three main avenues to find free COVID-19 testing locations across the US: HRSA health centers, Test to Treat locations and ICATT testing sites. These options function similarly, but we'll break down the specific steps to find your nearest free testing location.HRSA health centers offer free COVID-19 testing
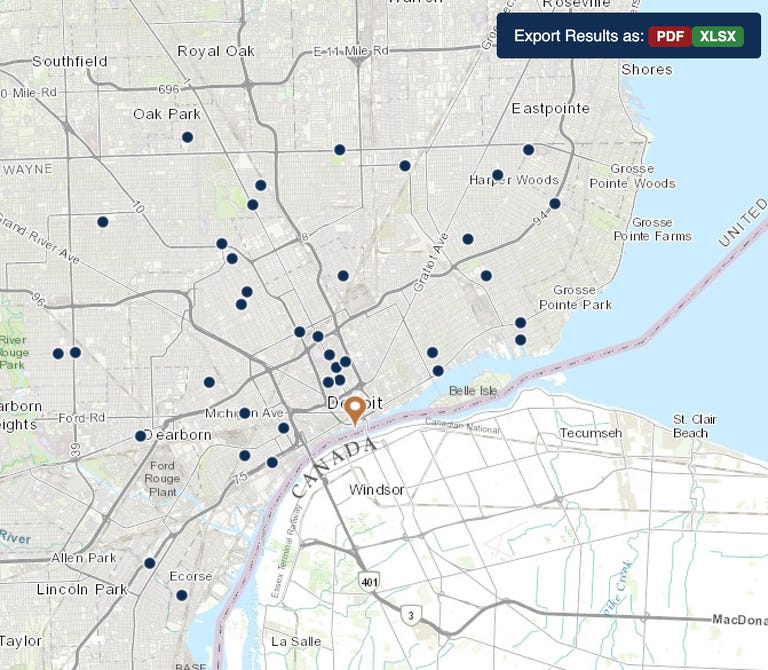
HRSA health centers offer free COVID-19 testing.
HRSA/Screenshot by CNET
The Health Resources and Services Administration funds health centers across the US. At these HRSA health centers, you will be able to receive free COVID-19 testing. You can use HRSA's locator tool to find a center near you.
First, select the language you would like to receive your results in. Then simply enter the location you wish to search into the box labeled Location. The locator also allows you to widen your search radius, so you can see all the options your area has to offer.
Once you've found a center that works for you, click through to that particular location's website and follow their specific instructions for obtaining a free COVID-19 test.
Test to Treat locations have COVID testing and medicine
The Test to Treat program makes COVID testing and therapeutics more accessible.
HHS/Screenshot by CNET
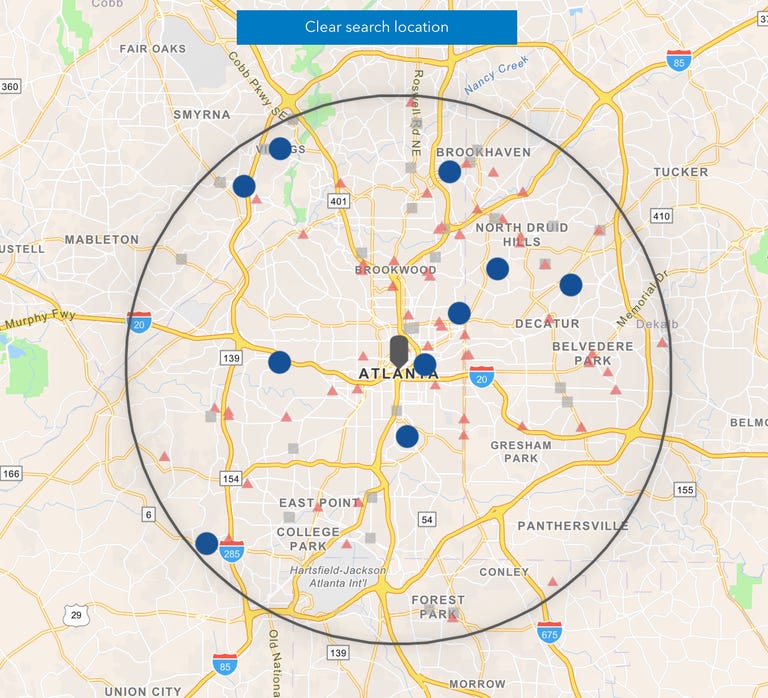
Test to Treat is a federally funded health care initiative that provides more accessible COVID-19 care. This option differs from the others in this article as you can use the Test to Treat centers to receive both COVID testing and treatment for infections. Like the other COVID-19 free testing options, Test to Treat has a locator tool that you can use to find an eligible Test to Treat center near you.
The Test to Treat center locator works like the other COVID testing search tools. Enter your location into the search bar and the tool will display Test to Treat locations in your area. A sliding bar lets you resize the search radius to capture all of the Test to Treat centers within your area.
Within the Test to Treat locator results, you'll be able to see each location's address, which COVID-19 therapeutics they offer and other special instructions you might need to know to get tested. If there's not an option to schedule a COVID test online through your chosen site, you may need to call.
Increasing Community Access to Testing provides COVID testing for the uninsured
ICATT offers free testing to uninsured patients who are showing symptoms of COVID-19 or who have recently been exposed.
CDC/Screenshot by CNET
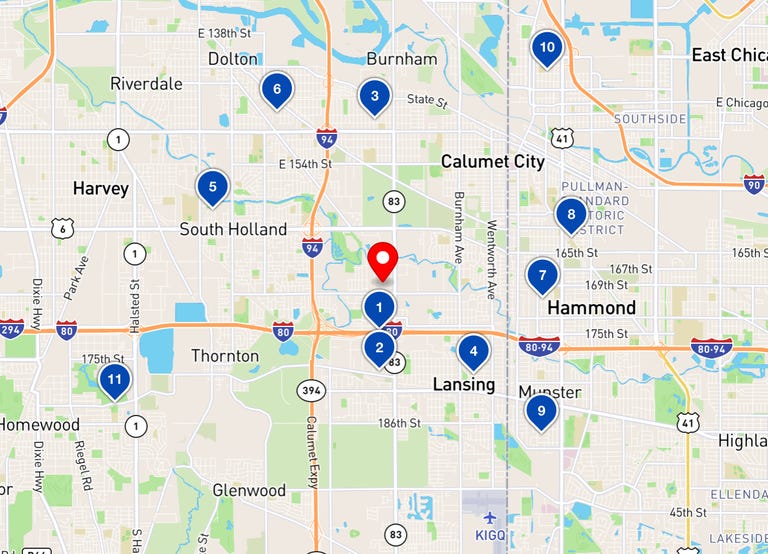
Increasing Community Access to Testing, or ICATT, is another free testing program that you can use if you need access to free COVID-19 testing. ICATT works a bit differently than the other programs on this list.
ICATT is specifically designed for uninsured patients who have been exposed to COVID-19 or are experiencing symptoms of COVID-19. Anyone can get an ICATT test at one of the program's locations, regardless of insurance status. If you are uninsured and you wish to be tested at an ICATT-eligible site, you will not need to pay for your test. If you are insured, you might need to pay a fee.
The ICATT locator tool works just like the other locator tools for free COVID testing -- input your address or your ZIP code to find ICATT locations near you. There is a search radius adjuster in this locator to tweak your searches to capture the entire area that you want to search.
Once you've found a location, follow your testing site's steps for scheduling your appointment.
How can I get free COVID-19 vaccines and booster shots?
COVID-19 vaccines and boosters are an important protection against contracting or getting seriously ill from the virus. Since the CDC has recommended updated COVID-19 booster shots for everyone 6 months or older, you might be wondering how to find free COVID-19 vaccines.If you don't have insurance or a health provider, don't worry. The Department of Health and Human Services website says, "COVID-19 vaccines are 100% free for every individual living in the United States."
On Sept. 14, the Department of Health and Human Services launched the Bridge Access Program, which will continue to provide free vaccines to those who are uninsured through local health departments and HRSA centers. CDC has also partnered with "more than 20,000 retail pharmacy locations nationwide" to provide free vaccines by modifying the existing ICATT program mentioned above.
The Bridge Access Program will end in December 2024, but until then, you'll be able to access free COVID-19 vaccines. To use it, go to vaccines.gov, choose which shot you want, and then click the "search" button. On the next page, select the option that says "Bridge Access Program Participant" to show which locations offer no-cost vaccines.
For more, learn how your blood type could make you more susceptible to COVID and everything to know about the updated COVID-19 boosters.
Correction, Sept. 21, 2023: An earlier version of this story contained incorrect information about the cost of vaccines for people without insurance. It has been updated with information about how people can get free vaccines.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,653
9 mins ago -News
The cure for long COVID may come from Ohio

- Share on facebook (opens in new window)
- Share on twitter (opens in new window)
- Share on linkedin (opens in new window)
- Share on nextdoor (opens in new window)
- Share on email (opens in new window)

Illustration: Shoshana Gordon/Axios
Ohio State researchers are working toward a cure for long COVID, supported by the school's largest grant ever received for an infectious diseases study.
Why it matters: Long COVID is a complex condition disabling millions of Americans that scientists have struggled to understand.
Zoom in: Nearly one-third of Ohioans once infected with the virus say they're still experiencing symptoms at least three months later, per census data.
- That can include fatigue, dizziness, chronic cough, chest pain, heart palpitations and gastrointestinal issues, National Institutes of Health (NIH) researchers say.
How it works: The study is focused on a specific enzyme that severe COVID patients' cells produce in high levels.
- Previous OSU research, which resulted in the grant award, found that mice lacking the enzyme are protected from early and late symptoms of COVID such as lung inflammation and blood clots.
- Now, researchers will work to develop techniques to target the enzyme in more cell types, with the goal of more effectively treating the disease..
- "It was the most disturbing experience of my life," she tells Axios via email. "To suddenly lose the ability to think, put ideas together, follow a simple conversation, was devastating. I am among the few fortunate patients who recovered after several months."
- That depends if an existing drug could be used to target the enzyme in question, Amer says, or if a new one would need to be developed and tested, which would take longer.
Mapped: Current COVID hotspots in the U.S.
COVID-19 wastewater viral activity levels
As of Aug. 1, 2024No dataMinimal or lowModerateHighVery high
A map showing COVID-19 wastewater viral activity levels by U.S. state. As of August 1, 2024, 44 states are showing high or very high levels of activity, 4 states are showing moderate levels, two states are is showing minimal or low levels, and one states are not reporting data.
Data: CDC; Map: Axios Visuals
A summer COVID-19 wave continues to impact most of the U.S. and Ohio is one of the states with high levels of virus activity, per the latest CDC data.
State of play: Virus activity has risen over the past month in the Midwest.
- While hospitalizations remain low, the surge poses a risk to the elderly, immunocompromised individuals and those with respiratory or cardiac conditions.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,654
Why COVID Cases Rise Every Summer | Johns Hopkins Bloomberg School of Public Health
Hot weather, human behavior patterns, and an easily mutating virus create the perfect recipe for COVID to peak in the summer.
Why COVID Surges in the Summer
Hot weather, human behavior patterns, and an easily mutating virus create the perfect recipe for COVID’s peak in the summer.Published
August 07, 2024
By Aliza Rosen
COVID-19
Infectious Diseases
Vaccines
Fall and winter are known as the time when respiratory viruses surge. When COVID emerged in 2020, it joined flu and RSV as one of the common respiratory viruses that peaks during the colder months. Since then, COVID has transitioned from pandemic to endemic, but has also maintained dual seasonality, peaking twice a year.
Every summer since 2020, COVID rates have risen in July and August, due to a confluence of virological, behavioral, and environmental factors. While it’s still too early to say whether this dual seasonality will peter out or become the norm, understanding why these summer surges happen can help us better protect against infection, severe disease, and ruined vacations.
Why do we see waves of COVID infections in the summer?
Several factors drive summer COVID waves. By mid-to-late summer, many people’s immunity—either from their last vaccination in the fall or from a previous infection—has waned considerably. That, combined with the emergence of more transmissible variants, makes the chance of infection more likely.
Human behavior also plays a major role. As the weather gets hot, we spend more time in air-conditioned indoor spaces, where most virus transmission occurs, explains Andy Pekosz, PhD, a professor in Molecular Microbiology and Immunology. With the windows closed to keep the cool air inside, we restrict ventilation and air circulation that has shown to reduce virus spread.
Many people travel more during the summer, with roughly half of Americans surveyed saying they planned to travel more, farther, and for longer in 2024 than the year prior. Travelers are not only exposed to more people—including from regions with more COVID cases—but also may be more likely to write off mild symptoms as simply the result of jet lag, not illness. Tiredness, headache, or a sore throat—all common after a long flight—are also symptoms of COVID, and without testing to be sure, a traveler may unknowingly expose others.
Pekosz experienced this himself after an international trip in July. At first he chalked up feeling tired to the massive time change, but when he started sneezing, he tested at home and it was positive. “I could have easily blown that off and just attributed everything to jet lag,” he says. “With a mildly symptomatic case, I may not have registered that it could be COVID and gone about my business for another couple of days while I was infectious.”
Why are there summer waves of COVID infections but not other respiratory illnesses like flu and RSV?
COVID’s ongoing dual seasonality can be attributed to both the higher presence of the virus year-round and its ability to mutate.
“The number of COVID cases that are present year-round is so much higher than we see for flu or RSV,” Pekosz explains. With that higher baseline, when conditions make for easier transmission—like increased travel and heat driving people indoors—there are more cases to fuel a larger wave of infections. “With flu or RSV, there are so few baseline cases during the summer that these changes in behavior don’t cause the same spread.”
Even when COVID rates are relatively low, more cases circulating year-round means more opportunities for the virus to mutate, which SARS-CoV-2 has proven to do very easily. When this happens, new variants emerge that are often more transmissible and better able to evade immunity. “The virus has shown itself to be very malleable, very able to handle mutations,” Pekosz says.
How might summer COVID waves impact our vaccination strategies?
The 2023-24 respiratory virus season marked a shift in COVID vaccination strategy in the U.S. to one of annual fall vaccination. That means that—just as with annual flu vaccines—governing bodies like the FDA and CDC use global surveillance data to predict which strains will be circulating and recommend a corresponding vaccine formulation. This happens in the spring so that manufacturers can prepare a vaccine for distribution in early fall.
But when infection rates increase, so do the chances for the virus to mutate. A wave of infections in the summer could result in new dominant variants that the vaccine may not protect against as effectively.
We saw this evolution play out in real time earlier this year. The FDA’s vaccine advisory panel was scheduled to meet in mid-May to make their recommendations for the fall, but they postponed the meeting to early June to allow more time to monitor the FLiRT variants that had recently become dominant in the U.S. On June 6, the FDA recommended monovalent JN.1-lineage vaccines, and then a week later updated their recommendations to a preference for the KP.2 strain, a member of the JN.1 family of variants.
“From a public health perspective, it would be great if we could send the same ‘go get your vaccines before respiratory season’ message at one time of year, with the updated vaccines timed to be available then,” Pekosz says. But consistent summer COVID waves could impact those recommendations. “It may end up that some individuals, particularly high risk individuals, are going to be urged to get vaccinated in early summer ahead of a presumed summer wave,” he says.
However, it’s unlikely that the upcoming season’s updated vaccines would be available by then, and those individuals would only have access to the previous season’s formulation. The previous season’s formulation would still provide some protection against severe disease and hospitalization, but it likely would have reduced effectiveness against newer variants.
Will COVID ever become seasonal like flu and RSV?
While the U.S. has experienced a wave of COVID cases every summer since 2020, it’s too early to say whether this is a long-term trend. Many public health experts still expect the virus’s annual spread will eventually look more like those of flu and RSV, which tend to peak during the winter. But exactly how long it will take to settle into that seasonal pattern is not clear.
“Historically, there are examples of viruses that do settle into a seasonal pattern after a transition period,” Pekosz says, pointing to the 1918 influenza pandemic, which he says took five or six years to take on the seasonal pattern we’ve come to expect. “We've got to hope that it'll settle into a more seasonal pattern, but we should also start thinking about strategies to deal with it if it doesn't.”
Can we expect COVID cases to drop before they rise again in the winter?
According to the CDC’s wastewater surveillance, COVID activity is high or very high in many states, with levels in the South and West nearing what they were in January. As students and teachers head back to school over the next few weeks, Pekosz expects cases will continue to spread before the fall vaccine formulation is rolled out.
While infection-induced immunity comes with higher risks than vaccine-induced immunity, this late summer wave will offer good population-level protection that will allow for case rates to trend back down. “I expect we’ll see a little bit of a lull starting around the middle of September or so, before we start seeing the late winter surge of COVID cases,” Pekosz says.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,655

COVID is spreading faster this summer in NJ. What's causing it?
NJ COVID-19 cases and hospitalizations have risen steadily from 165 in June to 509 this week, outpacing last summer and reflecting a nationwide trend.
COVID is spreading faster this summer in NJ. What's causing it?
2-minute read
NorthJersey.com
COVID-19 cases and hospitalizations have risen steadily since June in New Jersey, outpacing last summer’s numbers and reflecting a nationwide trend, state data shows.
But serious cases remain low in the state despite the increase in transmission. The number of COVID patients on ventilators has barely risen out of the single digits each day for much of the summer.
COVID numbers have been on the rise across the U.S., a trend that even saw President Joe Biden become infected in July. The numbers in New Jersey and nationally are still far below the annual peak in late December and early January each year, when transmission is greatest due to holiday travel and more time spent indoors together.
While experts thought COVID would behave as a seasonal virus such as influenza and RSV, that may no longer be the case, said Dr. Stanley Weiss, an infectious disease specialist at Rutgers New Jersey Medical School. The emergence of new variants — such as the KP.3.1.1 subvariant — where a strain of COVID mutates into a slightly different form, can cause transmission to increase regardless of the time of year.
"Our crystal balls have been very poor and part of that has been the rapid evolution of COVID variants," Weiss said. "They have been very unpredictable."
In New Jersey, there hasn’t been one dominant strain of COVID propelling the numbers this summer. As of late July, there were at least 12 subvariants of the Omicron strain circulating in New Jersey with one, LB.1, accounting for about 28% of cases, state Health Department data shows.
NJ COVID cases rose from 165 to 509
Another reason for the increase could be the weather. Despite some cooler temperatures this week, New Jersey is on pace to have one of its warmest summers on record. Heat and humidity usually forces people to seek air conditioner relief indoors where viral transmission is greater.Get the NJ Politics To The Point newsletter in your inbox.
A pithy, sometimes irreverent rundown on NJ politics and government.
Whatever the case, COVID hospitalizations in New Jersey were at 165 on June 1 and steadily rose throughout the summer to 509 as of Monday.
That's still far below the peak in daily COVID hospitalizations in New Jersey during the start of the pandemic, when more than 6,200 were hospitalized in April 2020, or during the Omicron spike, when nearly 6,100 were hospitalized in January 2021.
The number of new cases in New Jersey this summer rose to 2,910 as of Aug. 3 — about 1,100 more than at the same time last year. The number is likely far greater since the 2,910 count only includes those who tested positive with a PCR lab test, not a rapid home test.
Despite the rise, most cases are not serious. The number of COVID patients in intensive care statewide was 48 on Tuesday, about double the amount from early June. COVID patients on ventilators has remained constant. There were 11 as of Tuesday.
Although increasing rates in the summer could be a warning of an even worse fall and winter, updated vaccines from Pfizer, Moderna and Novavax will be available as soon as September to provide protection from the new variants.
The CDC recommends everyone ages 6 months and older, with some exceptions, to receive an updated 2024-2025 COVID-19 vaccine to protect against the disease, regardless of whether or not you have previously been vaccinated against the virus.
"The good news is these vaccines will offer better protection against the acquisition of COVID," Weiss said. "That could make a big difference in lowering transmission."
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,657

Covid Situation Report: Aug 8, 2024
Update on Covid providing information on prevalence and hospital admissions for England and its regions. This post is best viewed using the browser or Substack app.
Covid Situation Report: Aug 8, 2024
Update on Covid providing information on prevalence and hospital admissions for England and its regions. This post is best viewed using the browser or Substack app.

Bob Hawkins
Aug 08, 2024
8
1
Share
Introduction.
This report is part of a weekly series that summarises the Covid situation in England and its regions.A reminder that not all of the data previously included in the situation update is now available on a weekly basis. Where relevant, changes to the content and data sources have been noted.
This week the data published for England only covers case rates from the UKHSA Covid dashboard and daily Covid hospital information for July. As data for England is limited, I have also included the latest available data for Scotland, Wales and Northern Ireland. Finally, I summarise key points from the UKHSA statement on the Autumn 2024 Booster Vaccination published earlier this week.
Summary.
Recent data for England, Scotland, Wales, and Northern Ireland show a continuing decline in Covid levels, indicating the end of the latest wave.Over the past week, daily case rates in England have decreased again, signalling that the July wave is likely over. Case rates have dropped in nearly all regions except London, where they have remained stable.
In Scotland, hospital admissions and the number of beds occupied by Covid patients have been falling since the Summer peak, which was higher than the levels seen in Winter 2023/24. Although Covid levels in wastewater have significantly decreased, they remain relatively high.
Wales has seen a continued decrease in Covid cases and hospital admissions, indicating the likely end of the recent wave.
Northern Ireland is experiencing a similar trend, with hospital admissions for community-acquired Covid consistently declining from the latest peak.
Although the data indicates that this recent wave is almost certainly over, this is an important reminder that Covid is not presently a seasonal disease and may never become one. As such, we should anticipate potential future waves with the emergence of new variants and as immunity levels diminish.
With that in mind, the UK Health Security Agency has released the eligibility details for the Autumn 2024 booster campaign, which largely follows the criteria of previous autumn campaigns.
As always, it’s important to remember that the risk of hospitalisation from Covid infection increases significantly with age and for those immunocompromised. Also Long Covid remains a risk for all as shown by the recent ONS report. Therefore, it is prudent to take appropriate measures such as self-isolating when experiencing Covid symptoms and enhancing ventilation or wearing masks whenever possible.
For those who are interested, I recently published an article covering the ONS data on Long Covid in more detail which can be found here. Also a comprehensive review of the evidence in support of wearing masks is available here.
Status of main respiratory diseases in England.
The UKHSA National influenza and COVID-19 surveillance report has moved to a condensed summer report and is now released every two weeks. Consequently, there is no updated information on Covid test positivity or weekly hospital admissions available to report. The next update will be published on Thursday, August 15.
Covid case rates in England
The UKHSA Covid dashboard continues to publish daily case rates for England on a weekly basis. As the majority of testing now occurs in hospitals or under medical supervision, these rates should closely align with hospital admissions. However, a comparison of daily case rates and daily admissions shows that this is not the case.Appendix 1 indicates that although Covid case rates typically reflect the pattern of hospital admissions, there is a notable discrepancy in the magnitude of changes, with admissions experiencing a more pronounced fluctuation than case rates. Therefore, while case rates are helpful in signalling the general trend of Covid within the population, they do not precisely represent the degree of change.
The first chart in this section shows daily case rate per 100,000 individuals.
The chart indicates that Covid case rates have peaked and have fallen for the past two weeks indicating that the ‘summer’ wave is likely over. Nonetheless, current case rates remain higher than those observed during the peak in May. It is important to note, as detailed above and in Appendix 1, that comparisons with the peak in Winter 2023 are not recommended.
The next panel chart in this section shows Covid rates for the regions of England. Hover your cursor over one of the chart lines to display the admission rates for all regions.
The panel charts indicate that daily case rates are declining in nearly all regions, except for London, where the rates have plateaued. Despite a recent decrease, the North East region still reports a case rate that is substantially higher than any other area.
Daily Covid hospital admissions and bed occupancy.
Starting April 2024, NHS England moved from a weekly to a monthly publication schedule for daily Covid data in hospitals. This section provides an overview of the most recent data, released on August 8, which covered the month of July. As a result, it does not include the most recent weeks data used in the prior section.The following chart illustrates the daily number of Covid hospital admissions, including patients diagnosed with Covid after admission, for the year 2024 up to the end of July, in comparison with the complete data for 2023.
The charts show that hospital admissions in Jun/Jul 2024 have increased above the equivalent levels seen in 2023. However, admissions in the last week of July 2024 are falling indicating a likely reduction in Covid levels in the community.
The next chart shows the daily number of beds occupied by Covid patients in 2024 compared with 2023. The number of beds occupied by Covid patients includes both those being treated primarily for Covid and those ‘with’ Covid as a secondary infection. As a guide, about 25% of patients occupying these beds were being treated primarily for Covid in March 2024.
Reassuringly, the data on hospital bed occupancy by Covid patients mirrors the pattern of Covid hospital admissions. This confirms the slight decrease in Covid levels see at the end of July.
In summary, the daily Covid hospital admissions and occupied bed data confirms the falls seen seen last week in the UKHSA weekly admissions data and the daily case rates presented in the previous section.
Scotland weekly hospital admissions and bed occupancy
Scotland continues to publish weekly data on hospital admissions and bed occupancy for Covid as well as waste water monitoring data. The dashboard for Scotland’s data can be accessed here.The following panel chart shows the most recent data for weekly Covid hospital admissions up to Jul 28, depicted in blue, together with the number of beds occupied by Covid patients up to Aug 4, shown in orange. The number of occupied beds represent patients being treated for Covid as well as those being treated with Covid.
The charts shows that the recent 'summer' Covid wave in Scotland has led to more hospital admissions and a greater number of beds occupied by Covid patients compared to the 'winter' wave. This contrasts with England, where 'summer' hospital admissions did not surpass those seen in 'winter'.
However, in the past three weeks Covid admissions and bed occupancy in Scotland has fallen quite quickly and this ‘summer’ wave appears to be over.
Scotland is now the only home nation that is monitoring Covid levels using wastewater sampling and the following chart shows the latest levels reported.
The data indicates that the Covid levels in wastewater detected during the recent 'summer' wave were higher than those observed in the 'winter' wave. This is consistent with the trend seen in the hospital data. Moreover, the latest wastewater data for week ending Jul 30 shows that levels are falling which again follows the trend seen in the hospital data.
Interestingly, the very high wastewater levels seen in summer 2023 did not correlate with very high hospital admissions. It’s difficult to say why this was the case but could be due to wastewater testing being less sensitive for the most recent variants.
Wales Covid cases and hospital admissions.
Public Health Wales publishes a weekly Covid dashboard, presenting key Covid hospital indicators for the preceding 90 days. This dashboard can be found here. Additionally, data regarding Covid cases detected through testing in hospitals and other medical facilities are released every week.The following charts shows the latest data for the weekly (7 day rolling sum) number of cases reported.
The chart shows that Covid cases in Wales are continuing to falling but remain high. This follows a surge in cases that surpassed the 'winter' wave and reached a peak that was the highest in over a year.
Data regarding Covid hospital admissions in Wales is published for the most recent 90-day period, and the following chart gives the current trend.
Hospital admissions for Covid increased in June, but have now fallen for the past four weeks, mirroring the trend observed in Covid cases, and confirming that the ‘summer’ wave is likely to be over.
Northern Ireland hospital admissions
Public Health Northern Ireland publishes a weekly COVID-19 Epidemiological Bulletin that provides data on Covid cases, hospital admissions and occupancy and care home incidents. The full report, published every Thursday, can be found here.The chart below presents the weekly count of Covid hospital admissions for cases where the infection was contracted in the community, thereby excluding patients who contracted Covid while in hospital. Note that hospital admissions data for the other home nations do include patients who were infected in hospital so should not be compared to the data for Northern Ireland.
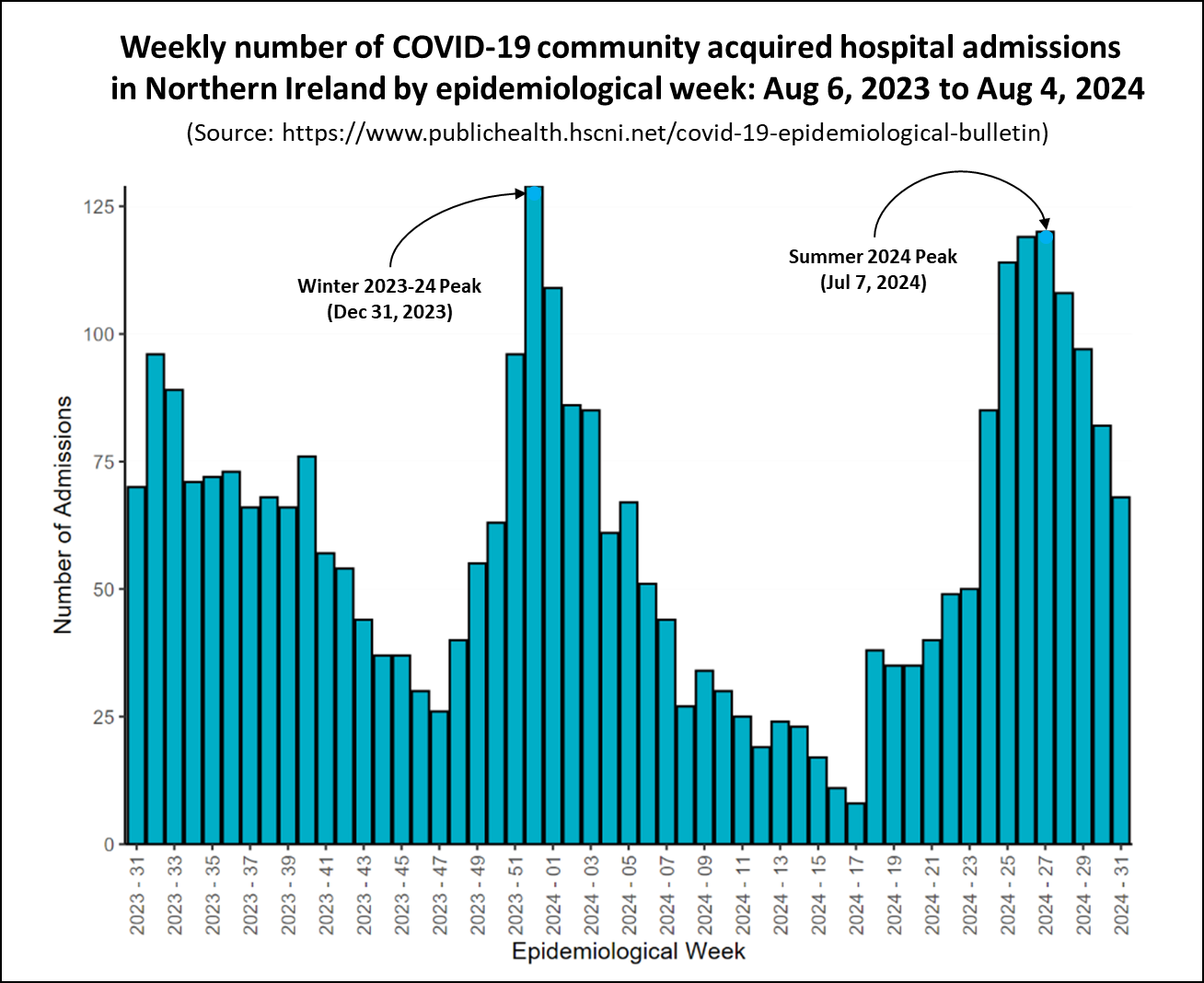
The chart shows a similar pattern to that seen in Scotland Wales, with the 'summer' wave's peak nearly reaching the heights of the 'winter' wave. However, a decline in admissions over the past four weeks suggests that the 'summer' wave is over.
Autumn 2024 Booster Vaccination Campaign
This week, the Joint Committee on Vaccination and Immunisation (JCVI), the UK government's independent advisory body on vaccines, released its advice for the Autumn 2024 Covid Booster vaccination campaign. This advice was considered by the UK Health Security Agency (UKHSA) who extended the JCVI list of those eligible to include other at risk groups.The JCVI advice, which can be accessed here, is grounded in a 'bespoke' cost effectiveness analysis, addressing both eligibility and the recommended vaccine products. As in their previous analyses, JCVI did not take Long Covid into account because they found that:
The JCVI cost effectiveness assessment for Autumn 2024 found that vaccination was likely to meet acceptable cost effectiveness criteria when offered to:“There remains considerable uncertainty regarding the impact of additional vaccine doses, beyond primary vaccination, on the risk, progression and/or outcome of post-COVID syndromes.”
- all adults aged 70 years and over;
- adults aged 65 years and over in a clinical risk group (excluding immunosuppression); and
- immunosuppressed individuals aged 15 years and over
The complete list of individuals eligible for the Autumn 2024 booster published by the UKHSA across all four nations of the UK are:
- adults aged 65 years and over;
- residents in a care home for older adults;
- individuals aged 6 months to 64 years in a clinical risk group;
- frontline NHS and social care workers: and
- those working in care homes for older people.
The UKHSA article acknowledges the difficulty in identifying individuals in the clinically at risk group, including those who are immunosuppressed, and offers additional guidance on this matter.
In conclusion
Although the amount of data currently being published has decreased, the limited information available for England suggests that although Covid levels are still higher than those seen in may they are now falling indicating an end to the ‘summer’ wave.Data from Scotland, Wales, and Northern Ireland suggest that the recent 'summer' wave of Covid saw higher levels than the 'winter' wave. Nevertheless, the most recent figures indicate that this surge has probably ended.
Lastly, the UK Health Security Agency has released the eligibility details for the Autumn 2024 booster campaign, which largely follows the criteria of previous autumn campaigns.
As always, if you have any comments on this Covid Situation Report or suggestions for topics to cover, please post a message below.
Subscribe
Appendix 1. How reliable are Daily Covid Case Rates?
The UKHSA Covid dashboard continues to publish daily case rates for England on a weekly basis. As the majority of testing now occurs in hospitals or under medical supervision, these rates should be closely aligned with hospital admissions and the positivity rate of tests.The first panel chart in this section tests that assumption by comparing the daily case rate per 100,000 individuals, shown in red, with daily hospital admissions for Covid reported by NHS England, depicted in blue.
The chart shows that while Covid case rates generally mirror the pattern of Covid hospital admissions, there is a significant disparity in the scale of changes. The grey shaded areas on each chart highlights the difference between the peak of the winter wave and the recent peak in June. Case rates experienced a 64% decrease, whereas hospital admissions saw a reduction of only 32% between the winter and June peaks.
In conclusion, although case rates are useful for indicating the overall trend of Covid in the population, they do not accurately reflect the extent of change. The likely reason for this is that testing levels have decreased by about a half since January.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,173
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,658

Noah Lyles tested positive for COVID-19 before winning bronze in men's 200
Noah Lyles left the Olympics arena in a wheelchair after winning the bronze medal in the men's 200 meters Thursday.
Noah Lyles tested positive for COVID-19 before winning bronze in men's 200
Tom SchadTyler DragonNancy ArmourUSA TODAY
SAINT-DENIS, France — Noah Lyles said Thursday night that he competed in the 200-meter final at the Paris Olympics while fighting COVID-19.
Lyles confirmed the news to reporters in the mixed zone after he didn’t win the 200 meters, which has long been his signature event. He wore a mask while speaking.
Lyles finished third behind Letsile Tebogo of Botswana and Kenny Bednarek, his U.S. teammate, in the 200. His time was 19.70. He said he tested positive for COVID-19 in the early morning hours of Tuesday.
Lyles, who has a history of asthma, laid on the track almost immediately after crossing the finish line, which is atypical of how he usually acts after a race. He needed medical attention shortly thereafter and, on the broadcast, soon collapsed into a wheelchair. He was talking with medical aides, which had oxygen handy, but Lyles did not appear to take it. He was wheeled off the track.

The Paris Olympics have been touted as the first Games to be held after the COVID-19 pandemic, but the disease has continued to infect athletes and impact the proceedings. A World Health Organization representative said earlier this week that at least 40 athletes had tested positive for the disease so far at the Games.
2024 Olympic medals: Who is leading the medal count? Follow along as we track the medals for every sport.

This story is developing and more details will be added as they become available.
Users who are viewing this thread
Total: 1 (members: 0, guests: 1)
Pakistan Defence Latest
-
-
A GIDS Shahpar II UAV of the PAF broke midair and crashed near Darya Khan, Punjab (5 Viewers)
- Latest: Broghil
-
-
-
Country Watch Latest
Latest Posts
-
-
Import Value of China-made EVs Soars by 848%, Making China the Top Import Country in south Korea (1 Viewer)
- Latest: Han Patriot
-
-

