Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
Elite Member
- Oct 2, 2013
- 64,167
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,103

STAGGERING: Australian Government Database Exposes Huge Death Toll from COVID Vaccines
The Australian government’s own database has exposed a huge death toll and staggering numbers of injuries from Covid vaccines...Where is the outrage? Where is the media?
Yommie
Elite Member
- Oct 2, 2013
- 64,167
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,108
Declaring COVID-19 “endemic,” Biden administration oversees policy of forced mass infection
The United States is currently mired in its ninth wave of mass infection since the start of the COVID-19 pandemic, with the population now completely abandoned by the powers that be.
www.wsws.org
Declaring COVID-19 “endemic,” Biden administration oversees policy of forced mass infection
Evan Blake@evanblake17
The United States is currently mired in its ninth wave of mass infection since the start of the COVID-19 pandemic, with the population now completely abandoned by the powers that be. A policy of forced infection has emerged, in which all public health measures have been scrapped and the most basic protection of mask-wearing is being criminalized in a growing number of counties and states.Wastewater data show that over 1.2 million Americans are being infected with COVID-19 every day. Hospitalizations are climbing, in particular among children and the elderly, while official deaths are approaching 1,000 per week. Excess deaths, a more accurate measure of the real death toll attributable to COVID-19, stand at over 500 per day, with the cumulative death toll in the US nearing 1.5 million. Long COVID, an array of symptoms which are often debilitating, now affects over 20 million Americans and over 400 million people globally.
According to wastewater modeler Dr. Mike Hoerger, there have been over 1.1 billion cumulative COVID-19 infections in the United States alone, with the average American infected three or four times. With multiple studies showing that each reinfection compounds one’s risk of Long COVID and other adverse health events such as strokes or heart attacks, the current trajectory of the “forever COVID” policy is towards ever-broadening mass debilitation and death on a world scale.
Under these conditions, on August 23 top officials from America’s leading public health agencies held an extraordinary press conference, which very explicitly outlined the Biden administration’s criminal “forever COVID” policy.
Leading the event was Centers for Disease Control and Prevention (CDC) Director Dr. Mandy Cohen, who bluntly declared that COVID-19 “is endemic, it is here with us.” This is the first time a top public health official has proclaimed COVID-19 to be “endemic,” after Drs. Anthony Fauci, Rochelle Walensky and Ashish Jha repeatedly and falsely said that the virus was “in the process” of becoming endemic since the emergence of the Omicron variant in late 2021.
An endemic disease is one which is largely contained, predictable and not disruptive to the basic functioning of society. None of this applies to COVID-19, which is spreading like wildfire almost year-round and causing widespread damage to the health of the population, as well as mass absenteeism and economic disruption to the tune of over $1 trillion annually.
After claiming that COVID-19 is “endemic,” Cohen hastened to add, “We need to protect ourselves. And we have the tools to do it, we just need to use them.”
Dr. Mandy Cohen, director of the U.S. Centers for Disease Control and Prevention since July 10, 2023 [AP Photo/Bryan Anderson]
The reality is that the public health “tools” necessary to mitigate the dangers of COVID-19, let alone stop the pandemic, have been systematically stigmatized, denied and even criminalized by the entire political establishment. The capitalist state, beholden to the profit interests of Wall Street and corporate America, has dismantled all pandemic surveillance and left the population to fend for themselves. Those who remain vigilant and seek to avoid infection are increasingly isolated and unable to protect themselves amid a sea of viral transmission.
Over the course of the press conference, it became abundantly clear that the only “tool” advocated by the Biden administration are new vaccines designed for the KP.2 variant, which are currently being rolled out. The officials present covered up the fact that these vaccines are too little, too late, given that the KP.3.1.1 variant is now dominant, with KP.2 accounting for just 3.2 percent of cases nationally, and that the current wave appears to be just peaking.
Furthermore, in the course of the press conference it became clear that the latest vaccines will not be guaranteed to everyone, with Cohen stating that uninsured Americans (over 26 million people) will have to try to navigate their local or county public health bureaucracy or pay upwards of $120 for the shot. No speaker seriously addressed the fact that vaccine uptake is abysmally low, the product of bipartisan anti-vaccine disinformation and propaganda portraying the pandemic as over.
Not once in the course of the press conference was the word “mask” even mentioned, despite the fact that numerous studies have proven that well-fitting N95 respirators can block the transmission of COVID-19 and all other airborne pathogens.
In fact, just two days after the CDC press conference, police arrested an 18-year-old in Nassau County, New York for wearing a ski mask after a county-wide mask ban was put in place earlier this month. Those arrested for wearing masks can face a fine of up to $1,000, up to a year in jail or both. A similar mask ban is now in effect in North Carolina, while cities, including Los Angeles, have floated the idea of such bans.
Another “tool” increasingly unavailable or impossible for average Americans to access is Paxlovid, one of the only effective treatments for COVID-19. In her remarks, Department of Health and Human Services (HHS) official Dawn O’Connell noted that starting in 2025, Pfizer will entirely control the distribution of Paxlovid. The pharmaceutical giant will undoubtedly charge the full price for the drug, which costs upwards of $1,500.
When asked by a reporter about the latest science on the risks of reinfection with COVID-19, Cohen downplayed the dangers and reiterated the vaccine-only strategy of the Biden administration, saying nothing about the need to wear masks to prevent transmission. The reality is that multiple studies have shown that each reinfection heightens one’s risk of developing Long COVID, which is only slightly mitigated by vaccination.
The response of the Biden administration to the latest wave of mass infection reaffirms that capitalism is descending into barbarism, with centuries of advances in science and public health trampled upon and discarded. Mass infection with a preventable illness is no longer to be prevented, but rather encouraged.
While the Democrats and Republicans bear primary responsibility for this policy of death, they are joined by the pseudo-left presidential campaigns of the Green Party’s Jill Stein and independent candidate Cornel West. Both have tailored their rhetoric to the far-right anti-vaccine constituency cultivated by Robert F. Kennedy, Jr., who himself has endorsed the “herd immunity” pioneer Donald Trump.
The only political party fighting for public health and science is the Socialist Equality Party and its candidates Joseph Kishore and Jerry White. Throughout their campaign, they have educated workers on the science of the pandemic, including the viability and necessity of a global elimination strategy towards COVID-19 and other pathogens. They have called for a vast infusion of resources to fund research into Long COVID and next-generation vaccines, as well as the renovation of all public spaces to ensure access to clean indoor air, to be paid for through the gargantuan military budget and the wealth of the financial oligarchy.
The policy of “forever COVID,” in which a virus known to damage every organ of the body is given free rein to cause perpetual reinfections in the entire global population, is not sustainable. No amount of rhetoric about COVID-19 becoming “endemic” will conceal the objective reality of declining health and well-being for masses of workers.
The essential task is to educate the international working class on the ongoing health dangers it confronts, which now coincide with the growing threat of nuclear war and fascist dictatorship, and to build a revolutionary socialist movement to put an end to the source of these scourges: the capitalist profit system.
Yommie
Elite Member
- Oct 2, 2013
- 64,167
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,110
Log in to Facebook
Log in to Facebook to start sharing and connecting with your friends, family and people you know.
 www.facebook.com
www.facebook.com
While the percent positivity in Ontario continues to rise, Ontario has not (publicly) reported cases for several months and also discontinued wastewater reports last month so these numbers may not be very accurate. The cases certainly are rising, though.
Ontario's current percent positivity is 15.6%. The last time the percentage was around this level was January 7 - 13, 2023 when it was 15.3%. There were 3,050 cases that week.
Yommie
Elite Member
- Oct 2, 2013
- 64,167
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,114

Why has COVID been so much worse this summer? The health belief model has the answer
Summer 2024 saw a big surge of COVID-19 cases. While COVID-19 is not the emergency it once was, it’s still a health threat, and we’d be wise to reduce our risk of getting it.
 theconversation.com
theconversation.com
Why has COVID been so much worse this summer? The health belief model has the answer
Published: September 2, 2024 8.33am EDTAuthor
 Jaigris Hodson
Jaigris Hodson
Associate Professor of Interdisciplinary Studies, Royal Roads University
Disclosure statement
Jaigris Hodson receives funding from the Social Sciences and Humanities Research Council. She is a resident fellow with the Cascade Institute and an advisor to the Clarity Foundation.Partners
Royal Roads University provides funding as a member of The Conversation CA.
Royal Roads University provides funding as a member of The Conversation CA-FR.
View all partners
Republish our articles for free, online or in print, under Creative Commons licence.
Republish this articleX (Twitter)
Facebook31
If you think COVID-19 was suddenly in the news a lot over the summer, you’re probably right.
Throughout August, outlets in both Canada and the United States ran headlines about high COVID levels, the summer surge of cases, timing of booster shots and reviving the use of face masks.
As numerous athletes tested positive for COVID at the Olympics in Paris, news outlets reminded Canadians that COVID is still a threat, and that summer cold symptoms might in fact be COVID.
The list of COVID news stories could go on and on, but what many experts seem to agree on is that this surge is a pretty big deal. In fact, Ashish Jha, dean of the Brown University School of Public Health predicts this wave might be the biggest summer surge since the virus started, according to an article in CNN.
Why COVID is surging now?

The Olympic rings are seen on the Eiffel Tower in July 2024 in Paris. Several athletes competed after testing positive for COVID-19. (AP Photo/Aurelien Morissard)
But why is the biggest surge occurring now, after health experts declared the end of the global health emergency over a year ago?
My research team at Royal Roads University studied how to share evidence-based health information during the COVID-19 pandemic, collecting interview, survey and experimental data between 2020 and 2023. We developed a framework that employed the health belief model for understanding why people may choose to act on health promoting behaviours — like adopting masks and vaccines during a pandemic.
Looking at the news about this latest surge, I think the health belief model can help people understand why our biggest summer surge has specifically occurred after the pandemic stage of the virus has been declared long over.
The health belief model
The health belief model helps public health practitioners and doctors understand what motivates people to adopt a positive health action (like quitting smoking or exercising), or act to reduce exposure to a negative health event (like getting a flu vaccine or practising safer sex).This model tells us that the likelihood of a person taking action towards a particular health outcome depends on the person’s perception of the risk of the negative health outcome to themselves personally, and also their perception of the benefit of the risk reducing behaviour. People also need to feel like they have the ability to take the necessary action, and that the action will be effective.
A summary of the health belief model can be seen in a diagram.
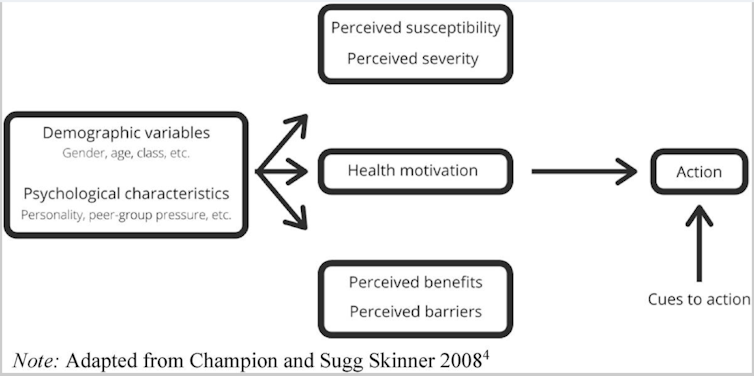
How the health belief model predicts what motivates people to adopt a positive health action (like quitting smoking or exercising), or act to reduce exposure to a negative health event (like getting a flu vaccine or practising safer sex). (S. Houlden et. al.), CC BY
Adopting the health belief model in practice means that public health communicators and the media need to illuminate both the risk of the negative health outcome, and the benefits and effectiveness of the risk reducing behaviours that will help people avoid the health danger. Both of these elements have been lacking since the end of the global emergency declaration for COVID-19.
Health belief and the summer of COVID
The reason I think we’re seeing such a surge now is because people don’t believe COVID is a risk, and they also don’t understand how getting vaccinations beyond the initial vaccine series from a few years ago would protect them now.When public health officials communicated the end to the global emergency stage of COVID, they unwittingly gave the public the impression that the danger was over. This decreased perceived risk and, with it, the likelihood that people would engage in regular vaccination, mask wearing and hand washing.
Furthermore, Health Canada no longer keeps or reports the latest COVID numbers, which means that many people have no real idea of the relative risk to themselves for gathering in public spaces, making them less likely to take precautions and more likely to pass on the virus.
Reporting on COVID in the media has not helped matters. While the dangers of new variants began to be reported as early as May of this year, the reporting on the spread of the virus didn’t really start to pick up until Olympians started collapsing after events.
Factors contributing to summer 2024’s big wave of COVID-19 include people being under-vaccinated and not taking other precautions like distancing or wearing masks. (Daniel Bockwoldt/dpa via AP)
This is the biggest summer wave because people are under-vaccinated and have stopped taking other precautions like distancing or wearing masks. And the reasons why we’re not taking these important risk-reduction behaviours is because many of us believe that COVID is over, or, if not over, that it’s not a big deal.
Read more: Making visible the invisible: Supporting long COVID patients and the people caring for them
But long COVID is still a risk and as of mid-August, the Public Health Agency of Canada reported over four million COVID cases in Canada. It’s not “just the flu” either, as with this summer surge, the World Health Organization also reports increases in hospitalizations.
COVID is not the emergency it once was, but it’s still a health threat, and we’d be wise to reduce our risk of getting it. That’s why public health communicators should re-integrate strategies that employ the health belief model to remind people that they are at risk, they can do something to reduce that risk and they will be better off for it.
Yommie
Elite Member
- Oct 2, 2013
- 64,167
- 37,187
- Country of Origin

- Country of Residence

- Thread starter
- #2,115

Long COVID symptom severity varies widely by age, gender, and socioeconomic status
Study analyzes self-reported long COVID symptoms through a healthcare app, revealing that symptom severity significantly varies by demographic factors such as age, gender, race, education, and socioeconomic status.
Long COVID symptom severity varies widely by age, gender, and socioeconomic status

In a recent study published in the journal JRSM Open, researchers analyze self-reported symptoms of long coronavirus disease 2019 (LC) from individuals using a healthcare app to examine the potential impact of demographic factors on the severity of symptoms. The researchers found that LC symptom severity varied significantly by age, gender, race, education, and socioeconomic status.
 Study: Long COVID symptoms and demographic associations: A retrospective case series study using healthcare application data. Image Credit: PeopleImages.com - Yuri A / Shutterstock.com
Study: Long COVID symptoms and demographic associations: A retrospective case series study using healthcare application data. Image Credit: PeopleImages.com - Yuri A / Shutterstock.comResearch highlights the urgent need for targeted interventions as age, gender, and social factors play a crucial role in the intensity of long COVID symptoms.
What factors increase the risk of long COVID?
Several months after recovering from coronavirus disease 2019 (COVID-19), patients with LC may continue to suffer from numerous symptoms, some of which include fatigue, brain fog, and chest pain. The prevalence of LC varies, with estimates ranging from 10-30% in non-hospitalized cases to 50-70% in hospitalized patients.Although several digital health interventions (DHIs) and applications have been developed to monitor acute symptoms of COVID-19, few have been designed to track long-term symptoms of the disease. One DHI called "Living With COVID Recovery" (LWCR) was initiated to help individuals manage LC by self-reporting symptoms and tracking their intensity. However, there remains a lack of evidence on the risk factors, characteristics, and predictors of LC, thereby limiting the accurate identification of high-risk patients to target preventive strategies.
About the study
In the present study, researchers investigate the prevalence and intensity of self-reported LC symptoms to analyze their potential relationship with demographic factors to inform targeted interventions and management strategies. To this end, LWCR was used to monitor and analyze self-reported LC symptoms from individuals in 31 LC clinics throughout England and Wales.The study included 1,008 participants who reported 1,604 unique symptoms. All patients provided informed consent for the use of their anonymized data for research.
Multiple linear regression analysis was used to explore the relationship between symptom intensity and factors such as time since registration, age, ethnicity, education, gender, and socioeconomic status through indices of multiple deprivation (IMD) on a scale of one to 10.
Education was classified into four levels denoted as NVQ 1-2, NVQ 3, NVQ 4, and NVQ 5, which reflected those who were least educated at A level, degree level, and postgraduate level, respectively. The intensity of symptoms was measured on a scale from zero to 10, with zero being the lowest and 10 the highest intensity. Descriptive statistics identified variations in symptom intensity across different demographic groups.
Study findings
Although 23% of patients experienced symptoms only once, 77% experienced symptoms multiple times. Corroborating with existing literature, the most prevalent symptoms included pain, neuropsychological issues, fatigue, and dyspnea, which affected 26.5%, 18.4%, 14.3%, and 7.4% of the cohort, respectively. Symptoms such as palpitations, light-headedness, insomnia, cough, diarrhea, and tinnitus were less prevalent.
Multiple linear regression analysis revealed that symptom intensity was significantly associated with age, gender, ethnicity, education, and IMD decile. More specifically, individuals 68 years of age and older reported higher symptom intensity by 32.5% and 86%, respectively. These findings align with existing literature that highlights the increased risk of LC symptoms with age, which may be due to weakened immunity or the presence of comorbidities. Thus, they emphasize the need for targeted interventions for this population.
Females also reported higher symptom intensity than males, by 9.2%. Non-White individuals experienced higher symptom intensity by 23.5% as compared to White individuals.
Individuals with higher education levels reported up to 47% reduced symptom intensity as compared to those with lower education levels. Higher IMD deciles, which reflect less deprived areas, were associated with lower symptom intensity; however, no significant association was observed between the number of symptoms reported and the IMD decile.
 Regression results with 95% confidence interval. Note: For age, the base group is people in the age category 18–27. For IMD, the base group is people from IMD decile 1. For education, the base group is people who left school before A-level (NVQ 1–2).
Regression results with 95% confidence interval. Note: For age, the base group is people in the age category 18–27. For IMD, the base group is people from IMD decile 1. For education, the base group is people who left school before A-level (NVQ 1–2).A significant positive association was observed between symptom intensity and the duration between registration on the app and initial symptom reporting. This finding suggests individuals may become more aware of their symptoms or that worsening symptoms prompt reporting.
Some limitations of the current study include the lack of data on comorbidities, hospitalization, and vaccine status. There is also a potential for bias against individuals lacking technological proficiency or access, which may affect the sample's representativeness, particularly for older, socioeconomically disadvantaged, or non-English-speaking individuals. Excluding patients with severe symptoms or those who were ineligible for the app may also skew the findings.
Conclusions
There remains an urgent need to develop targeted interventions to address the severity of LC in relation to age, ethnicity, and socioeconomic factors. LC treatment should prioritize prevalent symptoms like pain, neuropsychological issues, fatigue, and dyspnea while also considering other possible symptoms. Furthermore, sustained support for LC clinics is essential to effectively manage the wide range of symptoms and complexities associated with LC and improve public health outcomes in the post-pandemic era.Users who are viewing this thread
Total: 2 (members: 0, guests: 2)
Pakistan Defence Latest
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (10 Viewers)
- Latest: Bossman
-
-
Reports: Bajwa agreed to curtail Pakistan’s ballistic missile program (4 Viewers)
- Latest: Hakikat ve Hikmet
-
Country Watch Latest
Latest Posts
-
-
Indian general praises professionalism of Pakistani peacekeepers in South Sudan (10 Viewers)
- Latest: Bossman
-
-
-

