Yommie
SpeedLimited
- Oct 2, 2013
- 64,183
- 37,190
- Country of Origin

- Country of Residence

- Thread starter
- #1,351
Exercise May Ease COVID-19 and Long COVID Symptoms
Physical activity may help relieve certain acute and lasting symptoms of COVID-19 (especially mental and neurological symptoms)—at least for some people, according to recent research.
Exercise May Ease COVID-19 and Long COVID Symptoms

When you’re sick, exercise is usually the last thing on your mind. Simply engaging in your routine daily activities—much less intentional exercise—may feel impossible if you’re grappling with acute COVID-19 or Long COVID. But, surprisingly, recent research shows that physical activity might be the key to lessening certain acute and lasting symptoms of COVID-19 (especially mental and neurological symptoms)—at least for some people.
Following earlier studies showing that regular physical activity lowers risk of COVID-19 and Long COVID, researchers from Semmelweis University in Budapest, Hungary, investigated how regular exercise impacted COVID-19 and Long COVID symptoms in young women. This group was chosen to study because research has found that young women, in particular, have a higher prevalence of Long COVID.
Their findings, published earlier this year in Nature Scientific Reports, suggest that those who engaged in regular exercise fared better both when they were infected with SARS-CoV-2 and if they experienced subsequent Long COVID symptoms. But—and importantly—these findings may not hold true for those with post-exertional malaise (PEM), the defining characteristic of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and a persistent symptom of Long COVID.
The researchers conducted the study by asking 802 women aged 18-34 to complete surveys. The International Physical Activity Questionnaire Short Form (IPAQ-SF) was used to sort study participants into low, moderate, and high activity categories. The IPAQ form asks participants about their frequency of physical activity, defined as “moderate” (activities that make you breathe somewhat harder than normal) and “vigorous” (activities that make you breathe much harder than normal).
Women from each physical activity level were represented in the study: 43% of participants reported low levels, 35% moderate levels, and 22% high levels. For the highest level of physical activity, for example, one would need to climb stairs for 10 minutes, run for 20 minutes, or walk or cycle for 25 minutes daily. (You can read more details about the activity categories here.)
To assess the study participants’ COVID-19 history and symptoms, the researchers used the World Health Organization’s Post COVID Case Report Form. Fifty-five percent of study participants reported having COVID-19 (84% of which had a confirmed infection via a positive test). Around 90% of these patients had a mild severity COVID-19 infection, about 13% had a moderate infection, and 0.5% had a severe infection.
Regular exercise linked to fewer COVID-19 and Long COVID symptoms
Among the 50 different symptoms tracked in the study, over half of the participants reported fatigue, anxiety, dysmenorrhea (severe menstrual cramps), depressed mood, loss of interest/pleasure, and dizziness/lightheadedness during their COVID-19 infection. On average, patients reported 14 symptoms during acute COVID-19.
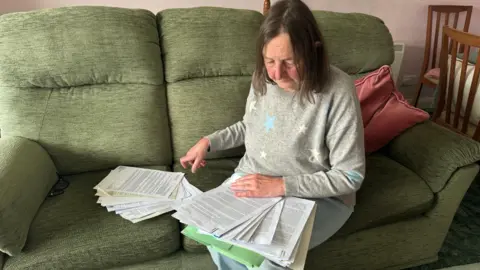
Credit: Jessica Stephen-Kuser
What’s interesting is that the number of symptoms reported decreased as physical activity went up: High-activity patients in the acute COVID-19 group had an average of 12 symptoms while low-activity patients reported 16. Moderate-activity patients were in the middle with an average of 13 symptoms.
In those who experienced Long COVID—a group that averaged 12 symptoms—the authors found a similar trend: High-activity groups reported fewer symptoms (an average of 8) compared to low- and moderate-activity groups (11, 14, respectively). In patients reporting Long COVID, 63% experienced fatigue and at least 40% of participants experienced one or more of the symptoms of dysmennorhea, loss of interest/pleasure, forgetfulness, anxiety, depression, palpitations, and/or trouble concentrating.
Reinfection (being infected more than once) was not correlated with participants’ level of physical activity.
The researchers hypothesize that the correlation of higher physical activity and fewer COVID-19 and Long COVID symptoms might be due to the known benefits that exercise and other forms of movement can have on the immune system. For instance, with Long COVID, specifically, increased cardiorespiratory fitness (how well your heart and lungs function) has been shown to reduce severity.
So far, except for people with post-exertional malaise, the evidence suggests the possibility that finding an exercise that you love and can do on a regular basis might help protect against a variety of symptoms caused by COVID-19 and Long COVID. However, it’s important to remember that this is not a one-size-fits-all approach and may not be suitable for some individuals.
Rhys Richmond is an MD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD:
One of my teachers, back when I was a resident, often said, "Exercise is the answer; what’s your question?" It was her way of saying that no matter what, exercise is good for you. Turns out to be particularly true for most people who get infected with the SARS-CoV-2 virus and those at risk for developing post-acute COVID syndrome. We already know that exercise is good for you. This study simply points out one more way it protects us.Unfortunately, it is very hard for patients who suffer from post-exertional malaise (PEM) to exercise. And yet, it is clear that not exercising at all allows another process to join with PEM to cause even more suffering—cardiovascular and muscular deconditioning. Deconditioning makes movement harder.
This doesn’t mean that patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and PEM should exercise. But they should try to integrate physical activity into their daily lives—to the extent that they can. It’s not easy. When you have ME/CFS and PEM, nothing is easy. But it is important. Patients with ME/CFS have limitations to the amount of energy they have to expend each day. Being active should be one of the many priorities they have—every day. It may be a small amount of activity, but some activity—within the limits they live in—will reduce the loss of muscle and strength and may end up making the other activities just a little easier.
Read other installments of Long COVID Dispatches here.
If you’d like to share your experience with Long COVID for possible use in a future post (under a pseudonym), write to us at: LongCovid[email protected]
Information provided in Yale Medicine content is for general informational purposes only. It should never be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.

















 Ahjané Forbes
Ahjané Forbes