Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,473

Virus that causes COVID-19 is widespread in wildlife, scientists find
SARS-CoV-2, the virus responsible for COVID-19, is widespread among wildlife species, according to Virginia Tech research published July 29, 2024 in Nature Communications. The virus was detected in six common backyard species, and antibodies indicating prior exposure to the virus were found in...
July 29, 2024
Virus that causes COVID-19 is widespread in wildlife, scientists find
by Matt Chittum, Virginia Tech
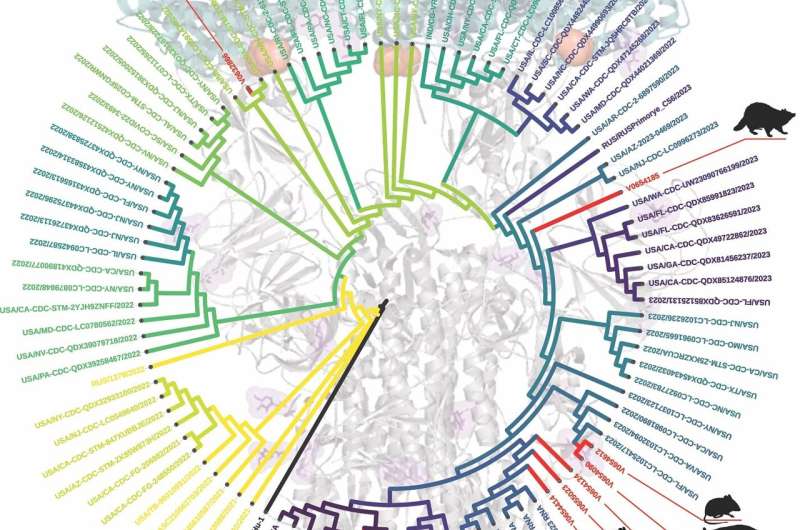
A Virginia Tech study of wildlife common in Virginia found that SARS-CoV-2, the virus responsible for COVID-19, is widespread in animals, particularly around areas of high human activity. The researchers identified variants consistent with those circulating in humans at the time, and one opossum with previously unreported viral mutations, underscoring the potential for changes that can potentially impact humans and their immune response. Credit: Joseph Hoyt/Virginia Tech
SARS-CoV-2, the virus responsible for COVID-19, is widespread among wildlife species, according to Virginia Tech research published July 29, 2024 in Nature Communications. The virus was detected in six common backyard species, and antibodies indicating prior exposure to the virus were found in five species, with rates of exposure ranging from 40 to 60% depending on the species.
Genetic tracking in wild animals confirmed both the presence of SARS-CoV-2 and the existence of unique viral mutations with lineages closely matching variants circulating in humans at the time, further supporting human-to-animal transmission, the study found.
The highest exposure to SARS CoV-2 was found in animals near hiking trails and high-traffic public areas, suggesting the virus passed from humans to wildlife, according to scientists at the Fralin Biomedical Research Institute at VTC, the Department of Biological Sciences in Virginia Tech's College of Science, and the Fralin Life Sciences Institute.
The findings highlight the identification of novel mutations in SARS-CoV-2 in wildlife and the need for broad surveillance, researchers say. These mutations could be more harmful and transmissible, creating challenges for vaccine development.
The scientists stressed, however, that they found no evidence of the virus being transmitted from animals to humans, and people should not fear typical interactions with wildlife.
Investigators tested animals from 23 common Virginia species for both active infections and antibodies indicating previous infections. They found signs of the virus in deer mice, Virginia opossums, raccoons, groundhogs, Eastern cottontail rabbits, and Eastern red bats. The virus isolated from one opossum showed viral mutations that were previously unreported and can potentially impact how the virus affects humans and their immune response.
Imagine a virus is like a key, and the cells it can infect are like locks. A virus can't infect any cell of any animal; it needs to find a cell with the right "lock" (called a receptor) or change its key (the viral proteins) to fit a new lock. To do this, a key needs to change shape by acquiring mutations to fit the new lock. This is what Carla Finkielstein and the Virginia Tech Molecular Diagnostic Lab at the Fralin Biomedical Research Institute noted with the keys present in SARS-CoV-2 when the virus jumped to wild species like opossums and squirrels. The key S-protein acquired at least two mutations, displayed in yellow in this simulation, that provided an evolutionary path for the virus to jump and transmit to other species. Credit: Carla Finkielstein/Virginia Tech
"The virus can jump from humans to wildlife when we are in contact with them, like a hitchhiker switching rides to a new, more suitable host," said Carla Finkielstein, professor of biological sciences at the Fralin Biomedical Research Institute at VTC and one of the paper's corresponding authors.
"The goal of the virus is to spread in order to survive. The virus aims to infect more humans, but vaccinations protect many humans. So, the virus turns to animals, adapting and mutating to thrive in the new hosts."
SARS CoV-2 infections were previously identified in wildlife, primarily in white-tailed deer and feral mink. The Virginia Tech study significantly expands the number of species examined and the understanding of virus transmission to and among wildlife. The data suggests exposure to the virus has been widespread in wildlife and that areas with high human activity may serve as points of contact for cross-species transmission.
"This study was really motivated by seeing a large, important gap in our knowledge about SARS-CoV-2 transmission in a broader wildlife community," said Joseph Hoyt, assistant professor of Biological Sciences in Virginia Tech's College of Science and corresponding author on the paper. "A lot of studies to date have focused on white-tailed deer, while what is happening in much of our common backyard wildlife remains unknown."
The research team collected 798 nasal and oral swabs across Virginia from animals either live-trapped in the field and released, or being treated by wildlife rehabilitation centers. The team also obtained 126 blood samples from six species. The locations were chosen to compare the presence of the virus in animals in sites with varying levels of human activity, from urban areas to remote wilderness.
The study also identified two mice at the same site on the same day with the exact same variant, indicating they either both got it from the same human, or one infected the other.
Researchers are not certain about the means of transmission from humans to animals. One possibility is wastewater, but the Virginia Tech scientists believe trash receptacles and discarded food are more likely sources.
"I think the big take home message is the virus is pretty ubiquitous," said Amanda Goldberg, a former postdoctoral associate in Hoyt's lab, who is the study's first author. "We found positives in a large suite of common backyard animals."
While this study focused on the state of Virginia, many of the species that tested positive are common wildlife found throughout North America. It is likely they are being exposed in other areas as well, and surveillance across a broader region is urgently needed, Hoyt said.
"The virus is indifferent to whether its host walks on two legs or four. Its primary objective is survival. Mutations that do not confer a survival or replication advantage to the virus will not persist and will eventually disappear," said Finkielstein, who is also director of the Virginia Tech Molecular Diagnostics Lab. The Roanoke lab was established in April 2020 to expand COVID-19 testing.
"We understood the critical importance of sequencing the genome of the virus infecting those species," Finkielstein said. "It was a monumental task that could only be accomplished by a talented group of molecular biologists, bioinformaticians, and modelers in a state-of-the-art facility. I am proud of my team and my collaborators, their professionalism, and everything they contributed to ensure our success."
Surveillance for these mutations should continue and not be dismissed, the scientists said. More research is needed about how the virus is transmitted from humans to wildlife, how it might spread within a species, and perhaps from one species to another.
"This study highlights the potentially large host range SARS-CoV-2 can have in nature and really how widespread it might be," Hoyt said. "There is a lot of work to be done to understand which species of wildlife, if any, will be important in the long-term maintenance of SARS-CoV-2 in humans."
"But what we've already learned," Finkielstein said, "is that SARS CoV-2 is not only a human problem, and that it takes a multidisciplinary team to address its impact on various species and ecosystems effectively."
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,474

COVID and Fibromyalgia: Is There a Link?
COVID may contribute to fibromyalgia or worsen one's symptoms. But further research is still needed to confirm this link.
COVID-19 and Fibromyalgia: Is There a Connection?
Researchers have theorized that COVID-19 may contribute to developing fibromyalgia or worsening one’s symptoms. But further research is still needed to confirm if there’s a link.
Many health conditions are connected. If one part of the body, like the brain or heart, is compromised, another part of the body can often be seriously affected.
As researchers search to understand these connections and what they mean for treatments, the question of whether COVID-19 and fibromyalgia are connected has risen.
Research in this area is ongoing, but it’s theorized that COVID-19 can contribute to the development or worsening of fibromyalgia symptoms. On the other hand, fibromyalgia alone may not lead to more severe COVID-19 symptoms.
Learn more about the connection between COVID-19 and fibromyalgia.
Is there a connection?
Fibromyalgia is a chronic condition that causes widespread pain in the muscles and soft tissue of the body, whereas COVID-19 is a highly contagious virus with many attributes of the flu. Both conditions can cause coughing, body aches, and trouble breathing or sleeping.ResearchersTrusted Source have theorized that COVID-19 may be able to contribute to the development of fibromyalgia or exacerbate (or worsen) an individual’s fibromyalgia symptoms.
The exact cause of fibromyalgia is not knownTrusted Source, but viral infections are thought to be a risk factor for triggering or worsening symptoms. Physical or mental stress is also a common factor that can lead to the development of or worsening of fibromyalgia, and COVID-19 is a well-known source of such stress.
Although many aspects of fibromyalgia aren’t fully understood, the central nervous system is known to play a critical role, and more than one-thirdTrusted Source of individuals have experienced their central nervous system being affected by COVID-19.
There’s speculationTrusted Source that long COVID may be linked to the development or worsening of fibromyalgia because it can cause inflammatory responses. Further research is still needed to fully understand the mechanisms of this, though.
There’s no evidence yetTrusted Source that fibromyalgia alone will put you at a greater risk of catching COVID-19, but if you have fibromyalgia and an associated condition that affects your immune system, you may be at a greater risk of COVID-19. You may also be at a greater riskTrusted Source of COVID-19 if you use immunosuppressant medications to help treat your fibromyalgia or related conditions.
Risk factors for fibromyalgia
The exact cause of fibromyalgia is not knownTrusted Source. But some risk factors have been identified:- Age: Older individuals are more likely to have it, as fibromyalgia is most commonly diagnosed in middle age.
- Gender: Women are also more likely to experience fibromyalgia than men.
- Other health conditions: Certain conditions, such as lupus and rheumatoid arthritis, are known to increase your likelihoodTrusted Source of developing fibromyalgia.
- stressful and traumatic events
- repeat injuries
- viral illnesses
- obesity
- a family history of fibromyalgia
Treatment options for fibromyalgia
Treatment for fibromyalgia may include a combination of medications, physical therapy, and alternative therapies.According to the Arthritis Foundation, a doctor may suggest treatment options such as:
- prescription medications like antiepileptics and antidepressants
- aerobic and muscle-strengthening exercises
- chronic pain support groups and classes
- stress relief techniques like meditating, journaling, and massage
- acupuncture
- therapy
- adopting good sleep habits
Can fibromyalgia be prevented?
Because the exact cause of fibromyalgia isn’t known, there’s no way to prevent it yet. But you may be able to lower the chances of a flare by:- taking steps to lower and manage your stress, such as meditating, journaling, and massage
- getting sufficient sleep
- eating a balanced diet
- avoiding alcohol
- not smoking
- exercising regularly
- attending support groups or therapy
When to speak with a doctor
It’s important to speak with a doctor if you don’t have a diagnosis of long COVID or fibromyalgia and are experiencing symptoms.You should also try to reach out to a doctor if your symptoms worsen or become severeTrusted Source. This may include:
- trouble staying alert
- worsening joint pain
- difficulty breathing
- persistent pain or pressure in the chest
- difficulty concentrating and remembering information
- pale, blue, or gray-colored skin and lips
Frequently asked questions
What
Because fibromyalgia isn’t a life threatening condition, it’s unlikely to affect life expectancy.What worsens fibromyalgia pain?
Fibromyalgia pain can often worsen due to physical and emotional stress.Does COVID make fibromyalgia worse?
It’s still not clear whether COVID can make fibromyalgia worse. Further research is still needed to confirm a connection between the two conditions.ADVERTISING
Takeaway
It’s theorized that COVID-19 may be able to trigger the development of fibromyalgia and exacerbate the symptoms you experience. But fibromyalgia may not increase your risk of catching COVID-19 or worsen your symptoms.Some conditions commonly associated with fibromyalgia and the use of immunosuppressant medications can make you more vulnerable to COVID, though.
Research on COVID-19 is ongoing, so it’s possible that more connections between it and fibromyalgia will become clear in the future. If you’re experiencing either COVID-19 or a fibromyalgia flare, it’s important to speak with a doctor. They can help to advise you on the current best treatments.
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,475

Covid-19 sparking a new respiratory illness season
COVID-19 trends in the region remain consistent with last summer and this might be the new norm. Unlike Influe...
Covid-19 sparking a new respiratory illness season
By CJ GoaterJul 29, 2024 | 1:15 PM
Antonio Rubio / CC
COVID-19 trends in the region remain consistent with last summer and this might be the new norm.
Unlike Influenza, Covid does not appear to have an off-season, with cases popping up year-round.
“Normally your typical respiratory-type viruses, they don’t spread in the summer generally at all, it would be very rare that we would get for example an influenza report in the summer,” explained the Director of Health Protection and Chief Nursing Officer, Diana Gowanlock.
“Our levels are low, they’re pretty stable at a low level, but we’re still seeing COVID cases, whereas other respiratory viruses, often you wouldn’t see it, it would be absolutely nothing in the summer months.”
Before the pandemic respiratory illnesses adhered to seasons with little to no cases recorded after April or May and summer outbreaks being almost unheard of.
Covid has brought a new summer respiratory illness season to the table.
“It is still out there, so still the usual messages of, you know, staying home with your sick, definitely don’t go to a facility like a hospital or long-term care if you’re experiencing any kind of illness,” said Gowanlock. “Washing your hands, covering your mouth when you cough, all of those normal layers of protection, they’re all so important all year round.”
The risk of transmitting the illness is lower in the summer with more people spending time outdoors, but it remains present.
“It’s likely something we’re gonna deal with forever,” said Gowanlock. “The trends over the last few years, there’s not really a season, there’s a worse season and then a season that just continues.”
Yommie
SpeedLimited
- Oct 2, 2013
- 64,174
- 37,188
- Country of Origin

- Country of Residence

- Thread starter
- #1,479
:max_bytes(150000):strip_icc():focal(680x476:682x478)/TOUT-Jana-Kramer-Wedding-Exclusive-071424-3ee1d94069f043b6903011e05ab5c9bb.jpg)
Jana Kramer Says She’s ‘Pretty Sure’ Her Parents Caught COVID from Her Kids at Her Wedding
Jana Kramer revealed during the July 29 episode of her "Whine Down" podcast that days before her wedding with Allan Russell, their three children got sick with croup and likely COVID-19.
Jana Kramer Says She’s ‘Pretty Sure’ Her Parents Caught COVID from Her Kids at Her Wedding
The country singer explained on her 'Whine Down' podcast that her three children had COVID-19 and croup days before her and Allan Russell's July 13 weddingBy
Charna Flam
Updated on July 29, 2024 10:46PM EDT
0 seconds of 14 secondsVolume 0%
This ad will end in 5
Who Is Lady Gaga’s Fiancé? 3 Things to Know About Michael Polansky
CLOSE
:max_bytes(150000):strip_icc():focal(680x476:682x478):format(webp)/TOUT-Jana-Kramer-Wedding-Exclusive-071424-3ee1d94069f043b6903011e05ab5c9bb.jpg)
Allan Russell and Jana Kramer on July 13, 2024. PHOTO:
CRAIG AND EVA SANDERS PHOTOGRAPHY
Jana Kramer and now husband Allan Russell are recapping all the ups and downs of their Scotland wedding.
The country music star, 40, was joined by Russell, 43, on the Monday, July 29 episode of her Whine Down podcast, where she revealed that she's sure their children and parents all got COVID-19 days before the couple tied the knot. Kramer and Russell share son, Roman James, 4 months. Kramer also shares son Jace Joseph, 5, and daughter Jolie Rae, 8, with ex Mike Caussin.
Kramer confessed she wanted everything to be "perfect" when she and the Scottish soccer player exchanged their "I Dos" on Saturday, July 13, at Carnell Estate. The One Tree Hill alum added that one of her fears about the celebration was worrying if people would get sick.
Things went wrong immediately after Russell’s father picked their family up from the airport, where he was noticeably coughing, Kramer said. She added, “It wasn't solely him that was coughing. There were a lot of people coughing on the airplane to Glasgow.” But she explained that Russell’s father was “hacking up a lung” in a "little" car with poor ventilation.
Jana Kramer Marries Allan Russell in Scotland Wedding: See the Castle, Kilts and Tartan Ribbon Cake! (Exclusive Photos)
“In my mind I was thinking, 'It's fine, it's all good.' Then your dad says he has a fever like the next day,” she told Russell. “The next day, I heard [coughing sound] from Jolie, and I was like, ‘Oh, s---. Here we go.’ And then one hundred and four fevers later, all three kids were sick.”
She then confirmed that the children had croup and COVID. Kramer also said that her father Martin and mother Nora tested positive for COVID after they were with her three children. “So I'm pretty sure it was COVID.”
:max_bytes(150000):strip_icc():focal(542x515:544x517):format(webp)/Jana-Kramer-Wedding-Exclusive-071424-24-13364b243e6d4567a19b9f5ddd44e2ec.jpg)
Jolie Rae, Allan Russell, Roman James, Jace Joseph and Jana Kramer on July 13, 2024.
CRAIG AND EVA SANDERS PHOTOGRAPHY
“It was difficult because they were sick,” the singer confessed, explaining, that “a piece of [her] still wanted them to make awesome memories.”
Russell chimed in to explain, “There’s nothing that would have really changed. They just did it not feeling as good as they should have felt.”
:max_bytes(150000):strip_icc():focal(539x497:541x499):format(webp)/Jana-Kramer-Wedding-Exclusive-071424-23-76cd6c554beb4bd59c3daf7b005c0712.jpg)
Allan Russell and Jana Kramer on July 13, 2024.
CRAIG AND EVA SANDERS PHOTOGRAPHY
Jana Kramer's 3 Kids: All About Jolie, Jace and Roman
“I know, but that broke my heart,” the mother of three replied. “But I mean, we still got them out… because they wanted to too.” She confirmed the children didn’t go to Edinburgh because “that would be too much of a journey for them feeling sick.”
It was “so stressful” that the children’s fevers spiked on Wednesday, July 10, and Thursday, July 11, Kramer said, adding, “I regret at that moment not having help because it was just us.”
Never miss a story — sign up for PEOPLE's free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from celebrity news to compelling human interest stories.
Kramer explained that she felt anxious and worried she was going to get sick “for the big wedding day and then the honeymoon.” She continued, “So I then became like this insomniac for the rest of the vacation because I just would wake up with anxiety and then like a pool of sweat.”
“That was the piece of the trip that I felt bad for the kids. They weren't feeling good,” she said. "But again, looking back, they don't they don't remember that. They remember the castles, all the fun stuff.”
Users who are viewing this thread
Total: 1 (members: 0, guests: 1)
Pakistan Defence Latest
-
-
-
Bangladesh struggling to muster dollars to pay Indian power debts, sources say (4 Viewers)
- Latest: lightoftruth
-
Country Watch Latest
-
‘India is Broken: A People Betrayed' author estimates India needs 200 million jobs (8 Viewers)
- Latest: r3alist
-
-
-
-
India's forex exchange reserves expanded by $66 bn in 2024, at record high (4 Viewers)
- Latest: Circadian Rhythm
Latest Posts
-
-
Call from Dhaka, Colombo and Kathmandu for an end to Indian interference (14 Viewers)
- Latest: Rollno21
-
‘India is Broken: A People Betrayed' author estimates India needs 200 million jobs (8 Viewers)
- Latest: r3alist
-
