Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Covid-19 News and Discussions
- Thread starter Yommie
- Start date
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,863
Covid still high, mpox emergency, and parvovirus enters the chat
State of Affairs: August 20
Covid still high, mpox emergency, and parvovirus enters the chat
State of Affairs: August 20

Katelyn Jetelina
Aug 20, 2024
209
17
Share
Lots is happening in the public health world! Here’s your latest update.
Covid-19: Very high
Viral activity in wastewater—our best indicator of Covid–19 spread—is still “very high,” marking a very impressive summer wave. In fact, levels in the West are now the worst on record since the Omicron tsunami in 2021.There are signs of declining rates in the South and Midwest and a plateau in the West. However, recent wastewater signals can be unstable (look at that rollercoaster in the West below), so I’m not getting too excited yet.
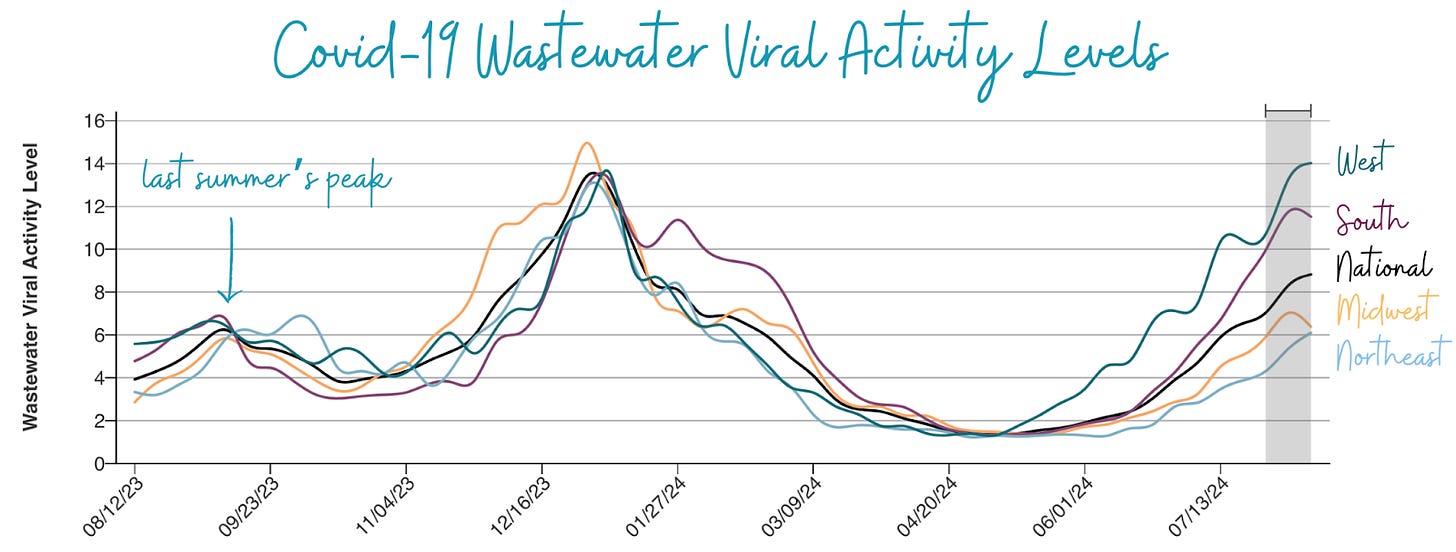
(Source: CDC; Annotations by YLE)
In addition, we are getting mixed signals from other metrics. Emergency department visits have shown signs of slowing down, but test positivity hasn’t yet.Hospitalizations are also increasing, which isn’t surprising given that it’s a lagging indicator, but levels remain lower than the winter peak. This past week, we lost 1,000 Americans to Covid-19.
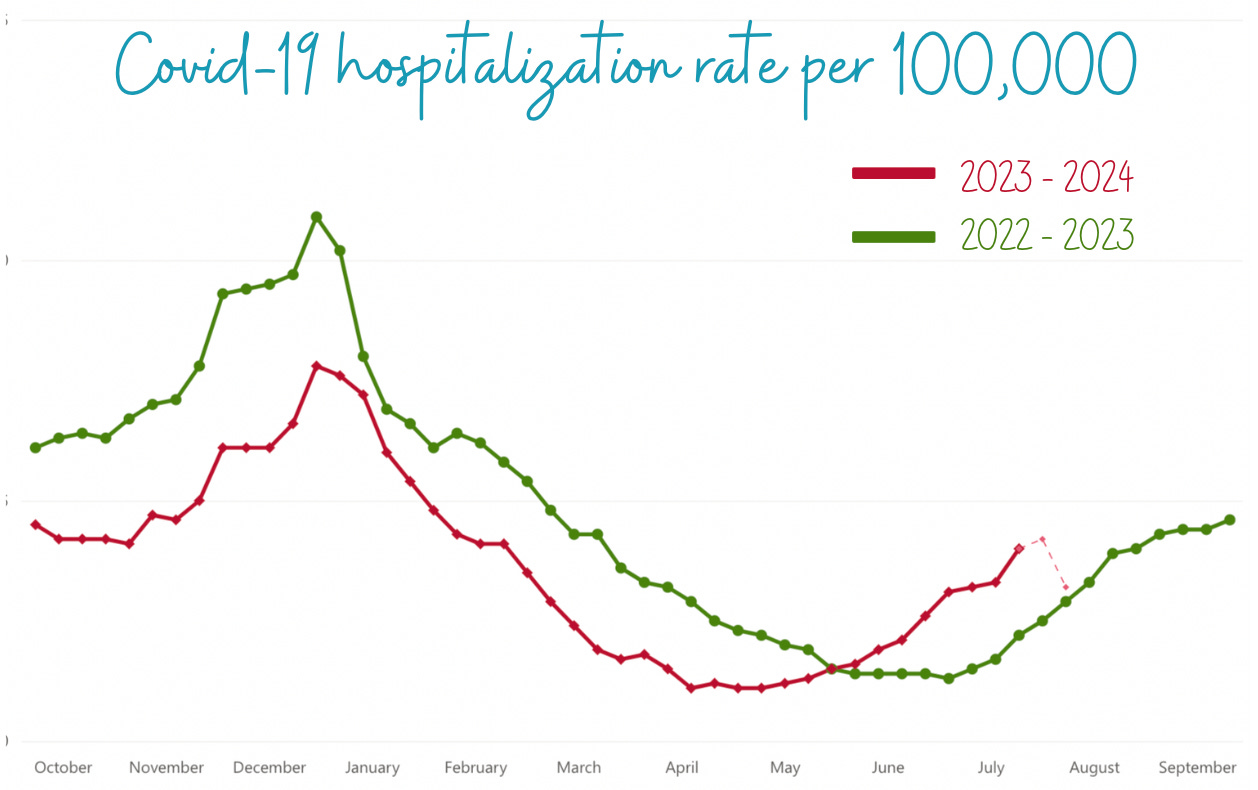
(Source: CDC; Annotations by YLE)
Note for the data gurus: Last April, hospitals were no longer required to report Covid-19 data, decreasing reporting from 90% to 38% of hospitals. However, there’s good news: Starting November 1, hospitals will report again! Thanks to all who submitted comments to Health and Human Services. It made a difference.
Mpox: An International Emergency
Last week, Africa CDC declared their first-ever public health emergency for mpox. The World Health Organization (WHO) followed by also declaring a public health emergency of international concern, signaling that the WHO Emergency Committee believes the current mpox outbreak in Africa is:- Unusual and unexpected
- Has the potential for cross-border transmission, and
- Requires coordinated international response.
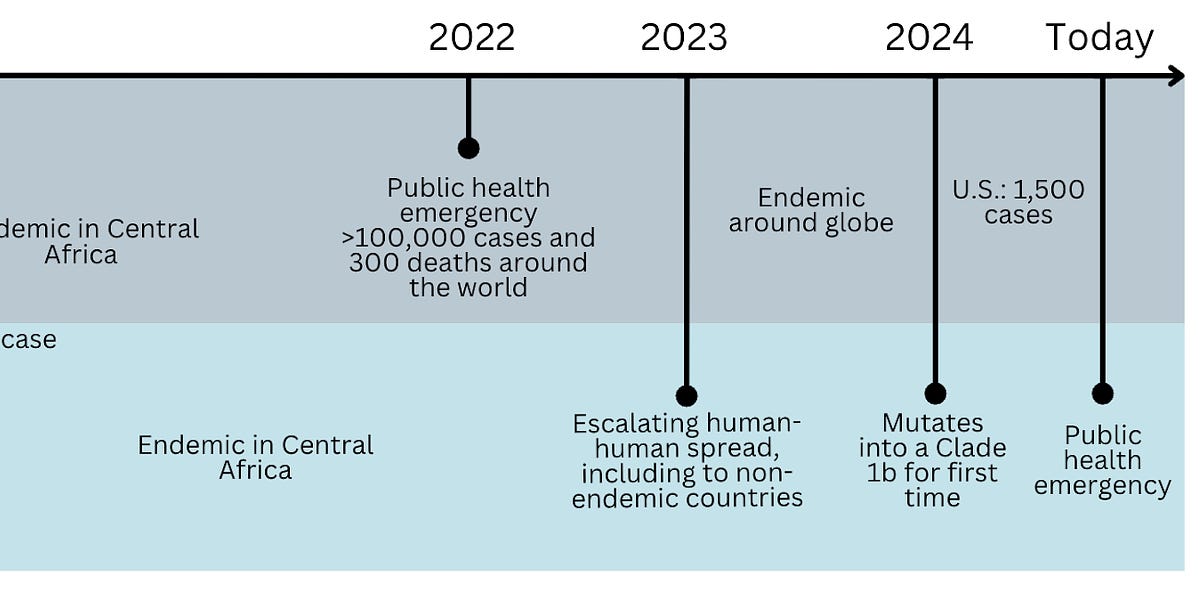
Back up—how did we get here? Mpox (formally known as monkeypox) has been endemic in Central Africa for decades, with rare, sporadic human cases of mpox after contact with infected animals.
However, in 2022, the virus—and specifically a strain considered less severe called Clade II—mutated and caused a massive international outbreak by spreading among a tight-knit social network: men who have sex with men (MSM). Education efforts, immunity, and antivirals have kept mpox spread low since. In 2024, the U.S. has had 1,657 cases of Clade II.
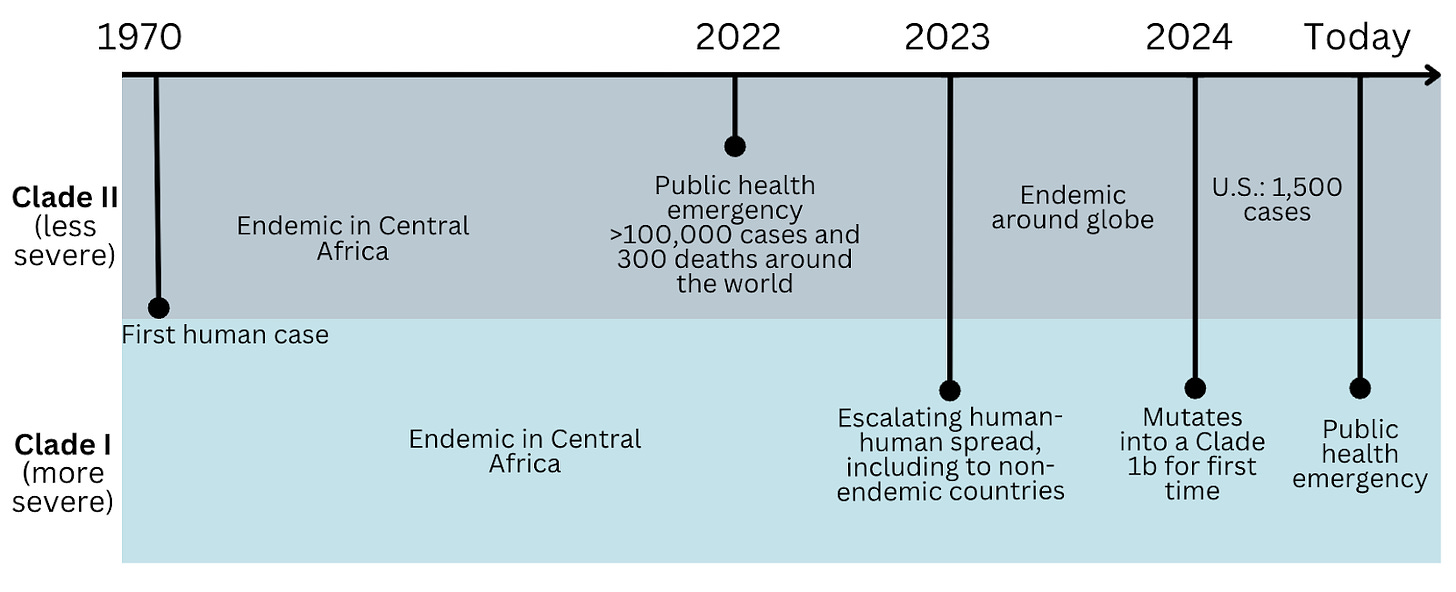
Figure by YLE
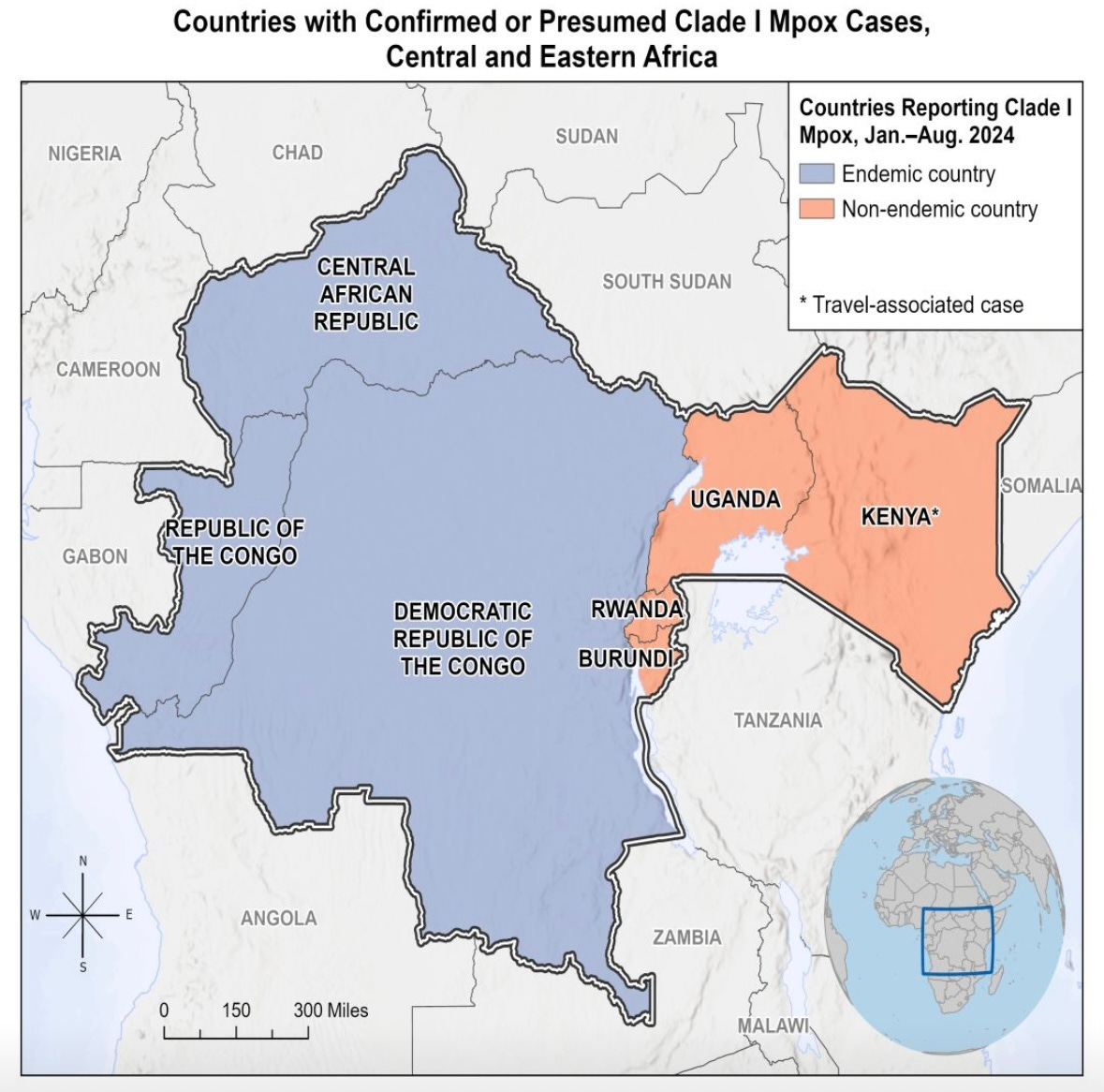
This brings us to today. Clade I—the other mpox strain, historically more severe—is now exploding in Africa, accounting for more than 17,400 cases and 500 deaths. (The true number is likely much higher due to significant under-detection and under-reporting.) Recently, Clade I has spread to non-endemic African countries, and over the weekend, 1 travel case was detected in Sweden.The majority of cases are the Clade Ia subvariant, with more than 80% of cases being among children and accounting for 85% of deaths. The second subvariant, Clade Ib, is spreading among adults.
No Clade I cases—regardless of subvariant—have been identified in the U.S.
What do we NOT know?
- What is Clade I’s dominant mode of transmission? There is overwhelming evidence that Clade II is spread through close contact, like sex. For Clade I, the at-risk population is different. Situation reports show transmission through multiple means: sexual contact, household contact, non-sexual contact (like healthcare exposures), and animal exposures. Experts on the ground do not see epidemiological evidence of airborne spread in Africa; they see, for example, cases of kids hunting squirrels or people in close contact in houses, like four kids in one bed. While there are documented cases of airborne transmission, what is possible isn’t always probable.
- How does the fatality rate apply to this Clade and other geographies? Historically, Clade I has a *very* high case fatality rate of 10% (compared to Clade II with <1%). However, it’s unclear whether this high rate is due to the intrinsic properties of the strain or is an artifact of under-detection, poor access to treatment, lack of healthcare, and poor nutrition in Africa. Data, such as an animal model and one small epidemiological study, have confirmed Clade I is more genetically virulent.
- How effective is TPOXX (the antiviral) against Clade I? A recent study in the Democratic Republic of the Congo found that while TPOXX was safe, it did not significantly shorten the duration of pox lesions in Clade I cases. The overall death rate and lesion duration among participants were lower than expected among all participants regardless of whether they received TPOXX or placebo, likely due to the high-quality care provided during the trial.
- How big will this outbreak be? Due to travel routes, we expect more international cases, especially in European countries. According to CDC modeling, any outbreak of mpox Clade I is expected to be smaller among the MSM community than the 2022 mpox Clade II outbreak.
So, what are we supposed to do? What matters now is that African countries can access vaccines, treatments, and the resources to run important studies to stop this epidemic.
In the U.S., only Clade II is spreading, so those eligible for the mpox vaccine have not changed: gay, bisexual, and other men who have sex with men, transgender or nonbinary people. Make sure you get both doses to be fully protected. For everyone else, there’s nothing to do for now.
Parvovirus B19: Increasing
In the U.S., parvovirus B19—a very common airborne respiratory virus, also known as fifth disease or “slapped cheek” rash—has increased to higher than “normal” in recent months, particularly in children ages 5 to 9. CDC urged physicians to be on the lookout.The exact reason for the current rise is unknown, but the virus typically spikes every 3-4 years, usually as it starts to warm (late winter to early summer).

Image: Mayo Clinic
Importantly, this virus is not dangerous to the general public. In fact, 50% of people have immunity by the time people reach 20 years old. However, three groups are at high risk because the virus attacks the cells that make red blood cells. This can result in short-lived anemia before the immune system controls the infection.- Pregnant: The virus can cause heart failure in the fetus and miscarriage.
- Immunocompromised: The anemia can be long-lasting.
- People with conditions that speed up the breakdown of red blood cells (like sickle cell): The anemia will likely be more severe and might require blood transfusions.
Bottom line
Covid-19 infections are still surging, and another virus—parvovirus B19—is also rising. There are things you can do—stay up to date on vaccines, mask indoors and in crowded areas, and get that indoor air flowing. Concurrently, the international community has another mpox emergency—for the U.S., though, those at high risk are still men who have sex with men. As always, we’ll keep you updated as things change.Love, the YLE Team
P.S. Thanks for all of your questions about fall vaccines! We are putting together a series of posts. Expect these in your inbox soon.
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,864

Ohio Gov. Mike DeWine tests positive for COVID-19
Gov. DeWine started experiencing mild, cold-like symptoms on Monday.
Ohio Gov. Mike DeWine tests positive for COVID-19
By Garrett Behanna
August 20, 2024 / 11:50 AM EDT / CBS Pittsburgh
COLUMBUS, Ohio (KDKA) -- Ohio Gov. Mike DeWine tested positive for COVID-19 on Tuesday, his office has announced in a press release.
Gov. DeWine started experiencing mild, cold-like symptoms on Monday. The governor took a cautionary test on Sunday before he developed any symptoms, and the test was negative.
He will work from home for the rest of the week.
KP.3.1.1, a variant in the Omicron family, is now the predominant COVID-19 variant circulating in the United States.
The CDC recommends COVID-19 vaccines for all people ages six months and older. Updated COVID-19 vaccines should be available in the early fall.
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,865

This year’s summer COVID wave is big; FDA may green-light COVID shots early
Wastewater SARS-CoV-2 levels suggest the summer surge is high and peaking right now.
going around —
This year’s summer COVID wave is big; FDA may green-light COVID shots early
Wastewater SARS-CoV-2 levels suggest the summer surge is high and peaking right now.
Beth Mole - 8/19/2024, 7:53 PM
Enlarge
Getty | Thomas Trutschel
154
With the country experiencing a relatively large summer wave of COVID-19, the Food and Drug Administration is considering signing off on this year's strain-matched COVID-19 vaccines as soon as this week, according to a report by CNN that cited unnamed officials familiar with the matter.
Last year, the FDA gave the green light for the 2023–2024 COVID shots on September 11, close to the peak of SARS-CoV-2 transmission in that year's summer wave. This year, the summer wave began earlier and, by some metrics, is peaking at much higher levels than in previous years.
Currently, wastewater detection of SARS-CoV-2 shows "very high" virus levels in 32 states and the District of Columbia. An additional 11 states are listed as having "high" levels. Looking at trends, the southern and western regions of the country are currently reporting SARS-CoV-2 levels in wastewater that rival the 2022–2023 and 2023–2024 winter waves, which both peaked at the very end of December.
Wastewater SARS-CoV-2 levels, by state.
CDC
Trends in wastewater SARS-CoV-2 levels by region over the last year.
CDC
Trends in wastewater SARS-CoV-2 levels by region for the entire pandemic.
CDC
Test positivity—a metric that has weakened given the dramatic decline in testing—shows a weekly test positivity rate of 18.1 percent for mid-August (amid a test volume of roughly 43,000). Such a rate, if truly reflective of cases, has not been seen since the initial towering omicron wave of January 2022, which peaked at 30.5 percent (with a test volume of roughly 991,000).
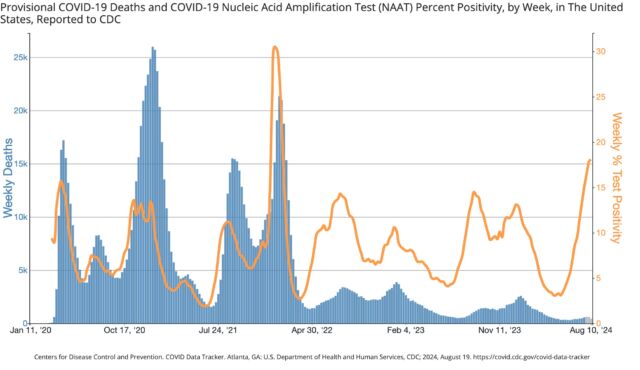
Enlarge / Test positivity in orange.
CDC
The good news is that given the substantial accumulation of protection from past infections and vaccinations, the two most serious metrics—emergency department visits and deaths—have not shown similar rises. The weekly percentage of emergency department visits with a COVID-19 diagnosis is low and similar to last year's summer wave. Deaths are likewise low, though they are still only provisional counts for the most recent weeks.
Ars Video
How Lighting Design In The Callisto Protocol Elevates The Horror
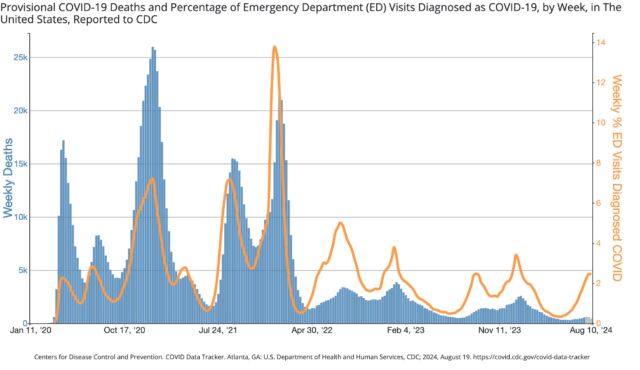
Enlarge / Emergency department (orange) visits and deaths (blue).
CDC
The FDA has firmly embraced a strategy to offer annual COVID-19 vaccines in the run-up to winter waves, not summer waves. The agency's thinking has always been to encourage Americans to get their flu and COVID-19 vaccines together between September and November, just before a mob of cold-weather respiratory illnesses strike together. The fresh vaccination boost can dull the levels of severe respiratory disease at a time when health care systems are most at risk of becoming overwhelmed.
Seasonality
But, while seasonal flu and some other respiratory viruses reliably surge almost exclusively in the winter, the seasonality of COVID-19 was never a given. And, so far, summer waves have arisen as consistently as winter ones, creating some awkwardness for the vaccine releases.Some experts have recommended getting a COVID-19 vaccine to protect against the summer surge. "Now is the time to get a dose with this surge," Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, told CNN on Sunday.
However, the only vaccines currently available target last year's strains (related to the XBB.1.5 omicron variant), which are long gone and may not offer strong protection against current strains (JN.1 and KP.2 omicron variants). Even if the 2024–2025 KP.2-targeting vaccine is approved by the FDA this week and hits pharmacy shelves next week, a dose takes two weeks to produce full protection. By that time, the summer wave will likely be declining. In fact, it looks to have already peaked in some parts of the country, including in some southern and western areas.
The other thing to consider is timing for maximum protection for the likely winter wave. For healthy people 5 years old and above, the CDC recommended getting only one shot last year. The shots offer peak protection for around four months. If you get your annual shot at the beginning of September, your protection may be on the decline if COVID-19 peaks again at the turn of the year, as it has the past two years.
According to the 2023–2024 guidance, people who are 65 and older can get a second COVID-19 booster four months after getting their first. People who are moderately or severely immunocompromised may also get additional doses of the updated COVID-19 vaccine.
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,869

The Invisible Damage: How COVID Rewires Our Brains
University of Colorado Boulder scientists have discovered that proteins left by COVID-19 can significantly lower cortisol levels in the brain, leading to heightened immune responses to new stressors. This research, focusing on the neurological symptoms of Long COVID, utilized rats to demonstrate
scitechdaily.com
The Invisible Damage: How COVID Rewires Our Brains
BY UNIVERSITY OF COLORADO AT BOULDERAUGUST 20, 20243 COMMENTS5 MINS READFacebookTwitterPinterestTelegram
SHARE

New findings indicate that residual COVID-19 proteins lower brain cortisol and intensify immune reactions, shedding light on Long COVID’s neurological symptoms. This study suggests that addressing these persistent antigens could help alleviate Long COVID symptoms. Credit: SciTechDaily.com
This research, focusing on the neurological symptoms of Long COVID, utilized rats to demonstrate how SARS-CoV-2 antigens persist in the body and alter brain function. This persistent effect could explain the severe and varied symptoms of Long COVID, suggesting potential directions for further research and symptom management strategies.
Understanding COVID-19’s Long-term Impact on the Brain
Proteins left behind by COVID-19 long after initial infection can cause cortisol levels in the brain to plummet, inflame the nervous system, and prime its immune cells to hyper-react when another stressor arises, according to new animal research by University of Colorado Boulder scientists.The study, published in the journal Brain Behavior and Immunity, sheds new light on what might underly the neurological symptoms of Long COVID, an intractable syndrome which impacts as many as 35% of those infected with the virus.
The findings come as COVID makes a striking summer comeback, with cases rising in 84 countries and numerous high-profile athletes at the Paris Olympics testing positive.
Cortisol’s Role in Long COVID Symptoms
“Our study suggests that low cortisol could be playing a key role in driving many of these physiological changes that people are experiencing with Long COVID,” said lead author Matthew Frank, PhD, a senior research associate with the Department of Psychology and Neuroscience at CU Boulder.Previous research has shown that SARS-CoV-2 antigens, immune-stimulating proteins shed by the virus that causes COVID-19, linger in the bloodstream of Long COVID patients as much as a year after infection. They’ve also been detected in the brains of COVID patients who have died.
To explore just how such antigens impact the brain and nervous system, the research team injected an antigen called S1 (a subunit of the “spike” protein) into the spinal fluid of rats and compared them to a control group.
Cortisol Reduction and Its Consequences
After 7 days, in rats exposed to S1, levels of the cortisol-like hormone corticosterone plummeted by 31% in the hippocampus, the region of the brain associated with memory, decision making, and learning. After 9 days, levels were down 37%.“Nine days is a long time in the life span of a rat,” said Frank, noting that rats live on average for two to three years.
He notes that cortisol is a critical anti-inflammatory, helps convert fuel into energy and is important for regulating blood pressure and the sleep-wake cycle and keeping the immune response to infection in check. One recent study showed that people with Long COVID tend to have low cortisol levels. So do people with chronic fatigue syndrome, research shows.
“Cortisol has so many beneficial properties that if it is reduced it can have a host of negative consequences,” said Frank.
Immune Response to Stressors in Exposed Rats
In another experiment, the researchers exposed different groups of rats to an immune stressor (a weakened bacteria) and observed their heart rate, temperature, and behavior as well as the activity of immune cells in the brain called glial cells.They found that the group of rats that had previously been exposed to the COVID protein S1 responded far more strongly to the stressor, with more pronounced changes in eating, drinking, behavior, core body temperature, and heart rate, more neuroinflammation and stronger activation of glial cells.
Implications for Long COVID Treatments
“We show for the first time that exposure to antigens left behind by this virus can actually change the immune response in the brain so that it overreacts to subsequent stressors or infection,” said Frank.He stresses that the study was in animals and that more research is necessary to determine whether and how low cortisol might lead to Long COVID symptoms in people.
But he theorizes that the process might go something like this: COVID antigens lower cortisol, which serves to keep inflammatory responses to stressors in check in the brain. Once a stressor arises – whether it be a bad day at work, a mild infection, or a hard workout – the brain’s inflammatory response is unleashed without those limits and serious symptoms come screaming back.
Those might include, fatigue, depression, brain fog, insomnia, and memory problems. Frank said he is doubtful that cortisol treatments alone could be an effective treatment for Long COVID, as they would not get at the root cause and come with a host of side effects. Instead, the findings suggest that identifying and minimizing different stressors might help manage symptoms.
Searching for Solutions
Rooting out the source of antigens –including tissue reservoirs where bits of virus continue to hide out – might also be an approach worth exploring, he suggests.The study was funded by the nonprofit PolyBio Research Foundation. More research is underway.
“There are many individuals out there suffering from this debilitating syndrome. This research gets us closer to understanding what, neurobiologically, is going on and how cortisol may be playing a role,” said Frank.
Reference: “SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids” by Matthew G. Frank, Jayson B. Ball, Shelby Hopkins, Tel Kelley, Angelina J. Kuzma, Robert S. Thompson, Monika Fleshner and Steven F. Maier, 21 July 2024, Brain, Behavior, and Immunity.
DOI: 10.1016/j.bbi.2024.07.034
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,871

The air travel issue no one wants to talk about
I’m sick of getting sick on planes. I got another case of COVID-19 last month, on a domestic flight, sitting near a woman who was sneezing.
OPINION
The air travel issue no one wants to talk about

Lee Tulloch
Travel columnistSave
Share
Normal text sizeLarger text sizeVery large text size
220
View all comments
Advertisement
Listen to this article
4 min
I’m sick of getting sick on planes.
I got another case of COVID-19 last month, on a domestic flight, sitting near a woman who was sneezing. I wore an N95 mask but she was wearing only the loose surgical type. I suspect she knew she was infectious.

Constant new variants put us all at risk.CREDIT:ISTOCKThere was nothing I could do about it. There were no seats to move into and, besides, to do so seemed a bit hysterical at the time.
Two days later – bingo. I wasn’t very ill, but I was visiting immune-compromised people and I put them at risk.
Nowadays, talking about masks – and indeed the virus itself – is deeply unsexy. They are a symbol of a past we’d rather not remember, even though that past is still our present and future while the disease keeps mutating.
But I still want to talk about masks because COVID-19 keeps happening to travellers, ruining holidays and causing potential long-term health issues, and yet airlines, government authorities and most passengers don’t want to know about it.
Just look around any flight. Or bus or train. Despite a few people clearly being sick, only a tiny percentage mask up. It’s not just as a precaution against COVID-19. There’s influenza, respiratory syncytial virus and other infections of a weakened immune system, which, perhaps unsurprisingly, can be caused by repeated COVID-19 infections.
Maybe COVID-19 is “just like a cold” and I shouldn’t fret. I certainly hope so because scientists are still learning about how each infection harms the body, with little idea what the consequences will be in three, 10 or 20 years.
I’m told I should “get over it”. But it’s not over with me.
4 min
I’m sick of getting sick on planes.
I got another case of COVID-19 last month, on a domestic flight, sitting near a woman who was sneezing. I wore an N95 mask but she was wearing only the loose surgical type. I suspect she knew she was infectious.

Constant new variants put us all at risk.CREDIT:ISTOCK
Two days later – bingo. I wasn’t very ill, but I was visiting immune-compromised people and I put them at risk.
Nowadays, talking about masks – and indeed the virus itself – is deeply unsexy. They are a symbol of a past we’d rather not remember, even though that past is still our present and future while the disease keeps mutating.
But I still want to talk about masks because COVID-19 keeps happening to travellers, ruining holidays and causing potential long-term health issues, and yet airlines, government authorities and most passengers don’t want to know about it.
Just look around any flight. Or bus or train. Despite a few people clearly being sick, only a tiny percentage mask up. It’s not just as a precaution against COVID-19. There’s influenza, respiratory syncytial virus and other infections of a weakened immune system, which, perhaps unsurprisingly, can be caused by repeated COVID-19 infections.
Maybe COVID-19 is “just like a cold” and I shouldn’t fret. I certainly hope so because scientists are still learning about how each infection harms the body, with little idea what the consequences will be in three, 10 or 20 years.
I’m told I should “get over it”. But it’s not over with me.
Advertisement
RELATED ARTICLE

Opinion
Tips & advice
Nervous flyers tense with fear during bumps. I know, because I am one
Lee Tulloch
Travel columnistThere’s massive public denial. Not many people bother to test these days. If you don’t test, you don’t know, so you’re free to assume you don’t have it. That’s certainly the skewed logic I’ve heard a lot lately.
So, if you’re masking on a flight, you’re in rare company.
During the pandemic, masks became a symbol of divisiveness, enraging sectors of our society who thought mask mandates took away personal freedoms. The freedom to get sick and infect others, I suppose.
I’m not quite sure what the humble, practical face mask did to deserve the controversy, despite being quietly worn for decades in Asian countries and by medical staff, but the culture war against it still rages.
It’s very possible, in certain societies, that if you wear a medical mask, you’ll have it ripped off your face or even get arrested.
RELATED ARTICLE

Opinion
Tips & advice
An airport is not a creche – don’t expect strangers to control your kids
Lee Tulloch
Travel columnistIn New York State, governor Kathy Hochul is considering a mask ban on subways, even as the city’s health department urges people to wear masks to combat an unprecedented rise in summer COVID-19 cases.
The laws are mostly directed at protesters who wear face coverings, and not people protecting themselves against disease. But the immunocompromised are angry that once again the mask has become the issue, not the behaviour.
Aerosol scientists conclude that N95 masks are 95 per cent efficient in blocking airborne particles. But over hours in a confined space, when you might have to lower your mask to drink, eat and sleep, they’re less effective, especially when the infected person isn’t masked properly too.
Currently, we rely on our fellow travellers being considerate. That’s a big ask. I suppose you could bring a few spare N95 respirators to distribute to passengers in your row as a precaution, but that might be misconstrued as rude.
But here’s the thing – I know if I get sick, my precautions haven’t worked. But it’s impossible to know how many other times I might have become ill if I hadn’t worn a mask to protect me.
So, even though the sight of me wearing a mask angers some people, and looks foolish to others, and even mentioning it drives people crazy, I’m sticking with the cover-up.
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,872
Letters to the Editor: We still need free COVID-19 tests. Why is it harder to get them?
Amid a summer COVID-19 surge, officials recommend testing. But readers say it's much harder to find free rapid tests.
Letters to the Editor: We still need free COVID-19 tests. Why is it harder to get them?

COVID-19 rapid tests are ready to be handed out at Tulita Elementary School in Redondo Beach in 2022.
(Jay L. Clendenin / Los Angeles Times)
Aug. 14, 2024 3 AM PT
To the editor: The excellent advice that people with symptoms should test themselves for COVID-19 (and thus limit transmission amid a persistent summer surge) would be easier to follow if the tests were cheaper to obtain.
My Medicare Advantage insurance (United Healthcare) will not cover the cost of buying a home test, even if prescribed by a doctor. The company treats it like any over-the-counter item.
At the same time, there is a great potential supply of tests. I still have a stack of tests with an FDA-extended expiration date of February or March 2024, and I suspect many other people do too. But the U.S. Food and Drug Administration has not reported further extensions of these dates for more than a year, suggesting no one has been checking. My tests still seem to work robustly well.
ADVERTISEMENT
I understand why the manufacturers have no incentive to do this. However, public health would be served if this supply of tests was utilized.
Public health would also be better served if the guidelines for when ill people can be around others were clearer and more consistent among various medical providers, many of whom, in my experience, consider the current guidelines from the U.S. Centers for Disease Control and Prevention too lax.
Carole Uhlaner, Irvine
ADVERTISEMENT
..
To the editor: In the face of the serious spike in COVID-19 cases, “officials recommend testing repeatedly over as many as five days after the onset of symptoms to be sure.”
That’s more than $50 worth of testing for one person, who may have to decide between testing and eating, paying rent, buying gas and getting school supplies for the fall.
What happened to free COVID-19 testing? And, why don’t you include that resource for your readers?
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,873
Tucker Carlson: Covid mRNA Vaccines Are ‘Poison’
Leading independent news reporter Tucker Carlson has warned that Covid mRNA shots are "poison."
Tucker Carlson: Covid mRNA Vaccines Are ‘Poison’
Leading independent news reporter Tucker Carlson has warned that Covid mRNA shots are "poison."

LIONESS OF JUDAH MINISTRY
AUG 20, 2024
84
23
Share
Exposing The Darkness is a reader-supported publication. To support my work, please consider becoming a paid subscriber.
Subscribe
One-time or recurring donations can be made through Ko-Fi:

Hunter Fielding August 19, 2024
Tucker Carlson has declared that Covid mRNA vaccines are “poison” and “toxic.”
During a new episode of his show, Carlson warns that the injections “clearly [don’t] work.”
He also revealed that he “personally” knows people whose lives were “destroyed” by the jabs.
Carlson described his decision to not get vaccinated as one of his “greatest achievements.”
“I think the vaccine is poison,” Carlson said before adding that he personally knows a couple who have had their lives destroyed by COVID shots.
“Whatever you think of how toxic it is, it clearly doesn’t work,” Carlson concluded.
“I do know a few people who developed heart conditions,” added Carlson’s guest, comedian Dave Smith.
“What we can say with 100% certainty is that the thing was sold on lies.”
WATCH:

Nearly four years after the debut of the so-called “vaccines,” it’s clear that people pushing the shots are not on the right side of history.
If people took six shots for polio and got polio three times, they would be asking some serious questions.
Source: newsaddicts.com
Yommie
Elite Member
- Oct 2, 2013
- 63,202
- 37,133
- Country of Origin

- Country of Residence

- Thread starter
- #1,874
From the Editor’s Desk: COVID Should Not Be the New Normal
ByCassandra Hemenway
-
August 21, 2024
https://www.facebook.com/sharer.php...tors-desk-covid-should-not-be-the-new-normal/
https://twitter.com/intent/tweet?te...should-not-be-the-new-normal/&via=montpbridge
 Cassandra Hemenway. Photo by John Lazenby.
Cassandra Hemenway. Photo by John Lazenby.This month, ragged from my first bout of COVID, I started to sit up a little straighter at mentions of long COVID. Anyone of any age is susceptible to it if they have had COVID even once, according to the National Institutes of Health.
It’s not surprising the virus caught up with me: Montpelier’s wastewater tests show high local SARS-CoV-2 virus levels; along with much of the nation, we are in a “surge.”
On Aug. 15, long COVID commentator Julia Doubleday wrote in her Substack, The Gauntlet, “… infectious disease modeler J.P. Weiland estimates that the US has yet again crossed the million-infections-per-day mark as of Aug. 9, with about one in 33 Americans currently infected with COVID-19.”
Doubleday laments that few public spaces now require COVID safety measures: “One in 33 means COVID in every restaurant, every supermarket, onboard every airplane, and of course in every hospital — where infection control teams continue to harm and kill vulnerable patients by failing to implement airborne infection control measures.”
“It’s just like a cold!” a young friend told me. Another emailed me to commiserate that I’d finally joined the annual summer COVID bout, for which she sets aside three weeks every year. Is that the new normal?!
It’s possible my encounter with COVID will begin and end with a few days of flulike symptoms, except I will be masking in public again and watching wastewater data. But for people who are immunocompromised, over 60, or have a variety of other conditions, COVID remains especially dangerous. And, as a woman, I am more susceptible to long COVID: About twice as many women as men get long COVID, according to the Centers for Disease Control and Prevention (CDC).
I live with three immunocompromised people, so when my visiting son and I both got COVID, we took care: we stuck to our isolation chambers, everyone in the house wore masks, we ran air filters 24/7, and we kept windows open despite the humidity and heat.
It was not the cheerful family visit we had anticipated. But it worked. The other three people in the household did not get infected. Still, with the threat of long COVID looming, I saw this as more than just a cold.
Little is known about long COVID. The CDC states on its website, it’s “a chronic condition that occurs after SARS-CoV-2 infection and is present for at least three months.” It can manifest with some 200 different symptoms, including severe fatigue, brain fog, and trouble standing up. It can become disabling, in some cases knocking people out of the workforce.
In June, the National Academies of Sciences, Engineering and Medicine released a 265-page report on long COVID, saying about 7% of U.S. residents have the condition and that most people contract it after a mild — not a severe — bout of COVID.
On Aug. 2, Sen. Bernie Sanders introduced a bill to study long COVID, the Long Covid Research Moonshot Act of 2024 (S.4964). Co-sponsored by U.S. Senators Tammy Duckworth (D-Ill), Tim Kaine (D-Va), Ed Markey (D-Miss), Tina Smith (D-Minn), and Peter Welch (D-Vt), it would provide $1 billion in annual funding for 10 years for long COVID research and treatment.
COVID is not the immediate existential crisis it was back in 2020 and 2021, but the global pandemic is not over. We’ve just stopped paying attention. COVID is still killing Americans routinely; according to the CDC, it was responsible for 1.9% of all deaths during the week ending Aug. 10. And the threat of long COVID is real.
My game plan was to never get COVID and therefore never have to worry I’d be one of the 7% of people the National Academies estimates end up with longer-term symptoms. That plan ended when I picked up my — unbeknownst to all of us — COVID-infected son from the airport. Asymptomatic people can and do transmit COVID, and within days, he tested positive and I got my first symptoms. Had we masked in the car, which would have been automatic a year or two ago, maybe only one of us would have gotten COVID. We were cavalier because we’ve been lulled into imagining the threat has subsided.
With millions of Americans currently struggling with long COVID, with the long-term effects so many new disabilities will have on our society, I have to wonder what’s next. I don’t know about you, but I didn’t sign up for that kind of normal.
Jenny Blair contributed to the reporting of this story.
Users who are viewing this thread
Total: 4 (members: 0, guests: 4)
Pakistan Defence Latest
-
-
NA-171 Rigging Scandal: PTI Voters Denied Entry as Armed Men Control Polling Stations (3 Viewers)
- Latest: Cash gk
-
-
-
AIR CHIEF CALLS ON TURKISH PRESIDENT AND MILITARY LEADERSHIP DURING HIS VISIT TO TURKIYE (4 Viewers)
- Latest: Zarvan
Country Watch Latest
-
Modernising the Bangladesh Air Force: time to turn away from China and Russia (10 Viewers)
- Latest: UKBengali
-
-
-
-
Latest Posts
-
Kamala Harris says Donald Trump ‘sold us out’ to China. He calls her a Marxist (2 Viewers)
- Latest: Yommie
-
-
-
SpaceX launch: Polaris Dawn crew looks to make history with civilian spacewalk (3 Viewers)
- Latest: Hamartia Antidote
-
Modernising the Bangladesh Air Force: time to turn away from China and Russia (10 Viewers)
- Latest: UKBengali