With key long COVID trials yet to yield results, people with the condition are trying to change how clinical trials are done.

www.nature.com
- NEWS FEATURE
- 02 April 2024
Long COVID still has no cure — so these patients are turning to research
With key long COVID trials yet to yield results, people with the condition are trying to change how clinical trials are done.
Lisa McCorkell co-founded a patient-led non-profit group to advise on research into long COVID. Credit: Marissa Leshnov for
Nature
When Lisa McCorkell got COVID-19 in March 2020, her symptoms were mild. Her physicians told her to isolate from others and that she would recover in a few weeks. But the weeks stretched into months and McCorkell, who was working on a master’s degree in public policy at the University of California, Berkeley, started having debilitating and bewildering symptoms: fatigue, dizziness and shortness of breath. Previously an avid runner, McCorkell found her heart racing from simple efforts.
She struggled to find an explanation, and soon realized that her physicians didn’t know any more about her condition than she did. To complicate matters, the limited availability of high-quality testing for the coronavirus SARS-CoV-2 in the early days of the pandemic left many of her doctors wondering whether her symptoms were really due to COVID-19 at all. “I didn’t have health-care providers that took me seriously,” McCorkell says. “That largely pushed me out of the health-care system.”
McCorkell turned instead to those who were experiencing the same puzzling symptoms and frustrations, joining a support group for people with what
would eventually be called long COVID. As they compared notes, McCorkell and a handful of others —
many of whom had research experience — realized that the information they were sharing might be helpful not only for those with long COVID, but also for those looking to study the condition. So, they founded a non-profit organization, called the Patient-Led Research Collaborative (PLRC), to design, provide advice on and even fund basic and clinical research into long COVID and other chronic illnesses.

Four years on: the career costs for scientists battling long COVID
A survey run by the group and published in 2021 catalogued the more than 200 symptoms experienced by people with the condition (
H. E. Davis et al. eClinicalMedicine 38, 101019; 2021). It is seen by some as
putting long COVID on the map. “They really jump-started the interest,” says Lucinda Bateman, a physician in Salt Lake City, Utah, who specializes in treating people who have long COVID and related conditions. “That was really a point from where more broad awareness arose.”
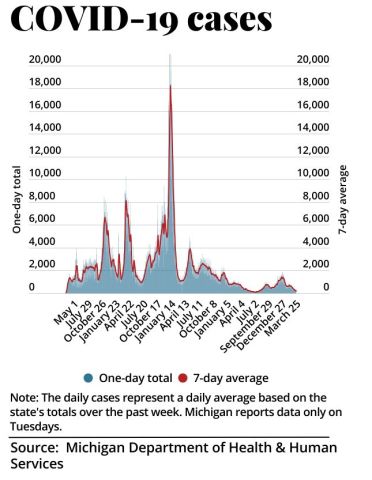
In the past few years, this study and similar patient-led efforts have helped to shape research programmes on long COVID and kick off some early clinical trials of therapies that might otherwise have gone unexplored. Many patient advocates see the efforts as crucial. They also think the results are more helpful for advancing the understanding of long COVID than the current findings from programmes funded by the US$1.15-billion RECOVER initiative led by the US National Institutes of Health (NIH). People with long COVID and their advocates have criticized the initiative for not always listening to the needs of people with long COVID.
Getting involved in research is challenging, given the symptoms of long COVID, but many patient advocates say they have no choice. “They’ve got you over a barrel,” says Margaret O’Hara, who coordinates patient involvement in research for a National Health Service hospital trust in England. O’Hara is on medical leave owing to long COVID. Referring to the research, she says: “You have to do it, because you are the one who is going to suffer for it if you don’t, but at the same time, you’re in bed sick.”
A plethora of symptoms
The PLRC’s survey of long COVID symptoms was the first major research study of the condition. The premise was simple enough: authors surveyed almost 3,800 people in 56 countries, many of whom were members of various long COVID support groups worldwide, including the network Body Politic, from which the PLRC originated. When the authors analysed the data, they found scores of symptoms in at least ten organ systems.
The study showed that the most prevalent problems were fatigue, post-exertional malaise — a worsening of symptoms after exertion — and the cognitive dysfunction that came to be
referred to as brain fog. Nearly 86% of participants reported relapses triggered by exertion; 87% said fatigue was a main symptom; and 88% reported brain fog, with no differences in cognitive issues across age groups.
The paper has amassed more than 1,000 citations, been mentioned in some 60 policy statements and is widely considered a seminal paper in long COVID research, owing to its in-depth analysis. For McCorkell, however, its impact is more fundamental. “What we demonstrated with the survey is that patients can lead high-quality research, and that it’s really necessary in order to have the most comprehensive look at a condition.”
The achievement is especially notable considering that the study was conducted by unpaid volunteers, most of whom identify as disabled, and it received no financial support. By contrast, many long COVID research initiatives have tended to focus on a subset of symptoms, which comes with the risk of missing the bigger picture, says McCorkell.
“There’s a lot of complexity in these illnesses, and I think it’s really important to embrace these complexities,” says Beth Pollack, a research scientist at the Massachusetts Institute of Technology in Cambridge, whose work focuses on understanding long COVID and other infection-associated chronic illnesses. With conditions that have a range of symptoms, and for which there is only limited research, building a knowledge base starts by listening to patients’ stories and capturing the nuances of their conditions, Pollack says.
Desperate measures
In early 2020, Martha Eckey, a pharmacist in Minneapolis, Minnesota, developed a COVID-like illness. She experienced a crushing fatigue that no amount of sleep could relieve, and was bedbound for days at a time. The physicians she went to for help had no answers. In desperation, Eckey turned to the online community of people with long COVID.
She found people trying treatments from prescription medications to over-the-counter supplements. But the effectiveness of these was restricted largely to personal anecdotes.
In the hope of getting a more comprehensive, systematic understanding of what worked, Eckey designed a survey called TREAT ME, which asked people with long COVID and those with myalgic encephalomyelitis, also known as chronic fatigue syndrome (ME/CFS), about their experiences, including whether they had tried any of a list of 150 medications and supplements.
More than 4,000 people responded.
Martha Eckey’s TREAT ME survey found overlap between treatments people were using for long COVID and for other chronic conditions.Credit: John Karp
Eckey found overlap with other chronic conditions. Some treatments revealed by the survey as most effective for long COVID were drugs such as beta blockers and the heart-failure medication Corlanor (ivabradine). These are sometimes used to treat postural orthostatic tachycardia syndrome, a nervous-system disorder that can be triggered by COVID-19. Eckey also found that a number of individuals reported relief after taking naltrexone, a non-opioid drug for treating substance-use disorder. When taken at low doses, it has anti-inflammatory and pain-relieving properties.
Physiotherapist David Putrino, who specializes in rehabilitation and human performance at the Icahn School of Medicine at Mount Sinai in New York City, says that the TREAT ME survey captured something both simple and profoundly important. “It’s a very fundamental question of, ‘what are you taking that’s helping right now?’” he says. The results have helped to guide his research on long COVID.
Listening to patients
TREAT ME attracted the attention of scientists and research foundations, who soon realized that this information could help to shape their efforts. One was the Open Medicine Foundation, a non-profit organization in Agoura Hills, California, that studies infection-associated chronic illnesses such as long COVID and ME/CFS.
Linda Tannenbaum, a clinical laboratory scientist, founded the Open Medicine Foundation in 2012 in response to the difficulties she encountered while seeking a diagnosis and treatment for her daughter, who has ME/CFS. Its first double-blind, randomized, placebo-controlled clinical trial will explore low-dose naltrexone (LDN) and another drug, pyridostigmine, which is used to treat an autoimmune disorder that affects voluntary muscle movements. The medications will be tested separately and in combination. Tannenbaum credits TREAT ME for helping to shape which symptoms will be assessed during the trial.
“The reason we are doing LDN as our first trial is that patients asked for it,” she says. TREAT ME also showed that many people with long COVID said that LDN helped to reduce brain fog (see
go.nature.com/3qy2tpj). Given these results, the Open Medicine Foundation also incorporated parameters in the trial to test cognitive function. Both LDN and pyridostigmine have been used to treat long COVID, but as many patients report, physicians are often reluctant to prescribe these drugs because of a lack of formal, randomized, controlled trials showing their effectiveness. “Doctors are very hesitant to go outside approved, or at least medically tested, medications,” says Bateman. In her experience, insurance companies also won’t pay for these medications for people with ME/CFS and long COVID without strong evidence to support their use.
Many patient advocates say that there is insufficient clinical research on the kinds of drug that people are already using. In February, the RECOVER initiative received a further $515 million over the next 4 years to test more interventions and investigate the long-term effects of a SARS-CoV-2 infection. But so far, the only trials it has begun are of the antiviral medication Paxlovid (nirmatrelvir and ritonavir), which started enrolling patients in July 2023, and of ivabradine and intravenous immunoglobulin, which recruited its first participants last month.
Lauren Nichols, a long COVID patient advocate, helped to lead the Body Politic support group.Credit: Lauren Owens Lambert/Reuters
RECOVER had come under fire for its plan to
test the effectiveness of a computer game for relieving brain fog, which critics say won’t meaningfully reduce symptoms, and for its decision to
plan an exercise trial, given that many people with long COVID experience post-exertional malaise.
“There are a lot of clinical trials that are focused on more behavioural and on non-pharmaceutical interventions, and that is really not a priority to the patient community,” McCorkell says. “It is a misunderstanding of how severe the condition is, and how much of an impact on people’s quality of life it has taken.”
A spokesperson for RECOVER told
Nature that the clinical trial of a computer game has already started enrolling participants and that the exercise trial is still scheduled to begin. They emphasized that these are accessible interventions, which might help some people who are affected, given the wide range of symptoms. They also said that moving these trials forwards will help in developing the framework for testing more treatments.
Lifting the fog
In the weeks after her initial COVID-19 infection, Hannah Davis found herself struggling with severe brain fog, to the point at which she could barely string two sentences together. Davis, who at the time was working as a data analyst and artist, with a particular focus on addressing biases in machine learning, kept waiting for her cognitive function to go back to normal, only for it never to return. “I had, and continue to have, terrible, terrible cognitive impairment,” says Davis, who is one of the co-founders of the PLRC.
Brain fog is having a significant impact on people’s livelihoods, says Wes Ely, a physician-scientist who works in intensive care at Vanderbilt University Medical Center in Nashville, Tennessee. People with long COVID have a form of cognitive impairment that is often “like mild and moderate dementia”, he says.
Ely, who studies treatments for Alzheimer’s disease and related dementias, decided in 2020 to expand into studying the cognitive impairments associated with long COVID. He quickly recognized that the condition is deeply complex, with symptoms that go beyond cognitive impairment.
To gain a comprehensive understanding of the phenomenon, he turned to the patient community, eventually recruiting Davis and Jaime Seltzer, director of scientific and medical outreach at the non-profit organization ME Action in Santa Monica, California. Together, they drafted a clinical trial to test the medication baricitinib, an immunomodulatory drug that is used to treat rheumatoid arthritis and alopecia areata, and acute COVID-19 infections. “I wanted to learn from people who are living with this disease,” says Ely.
The trio, along with other US investigators, designed a 550-person clinical trial of baricitinib as a potential treatment for long COVID. The trial has now been funded by the NIH and will start enrolment later this year.
From Seltzer’s perspective, an effective collaboration between patients and scientists can help both sides equally, because it leads to more effective and targeted research. “We have the resources to help you do what you do even better,” Seltzer says. The lived experiences of patients can shape research priorities in several key ways, she says. These include finding the most efficient way to allocate limited funds on the basis of symptom burden; offering context on the prevalence and severity of symptoms; and identifying how the trial design can capture improvement most effectively. All of this can help lead to faster breakthroughs in treatments, which is of benefit to both patients and researchers, Seltzer says.
Microclot mystery
In late autumn 2022, McCorkell flew to New York City to participate in a trial being conducted by Putrino and his team. This study aimed to look for the presence of tiny blood clots, called microclots, in people with long COVID. It is thought that these
cause symptoms such as fatigue and brain fog by impairing blood flow to the brain and body. There are still a lot of unknowns about microclots, including how many people with long COVID have them, how they form and whether the association is causal.

Long-COVID treatments: why the world is still waiting
McCorkell gave blood samples that were analysed using fluorescent microscopy, which confirmed she had microclots. McCorkell says it was “a wake-up call”. Until that point, she had been managing her symptoms mainly by avoiding overexertion. But the presence of the clots suggested to her that there might be active damage happening to her body. So, she started taking supplements that TREAT ME survey respondents reported as helpful.
Eckey’s results, which have not yet been published in a peer-reviewed journal, show that of 668 respondents with long COVID, between 40% and 70% found some symptom relief when taking the supplements nattokinase, serrapeptase or lumbrokinase, individually or in combination (see
go.nature.com/43xgyoq).
When Putrino saw these results, he decided it was crucial to conduct clinical trials of the supplements. He expects to begin a 120-person study on lumbrokinase in the coming months, and has involved patients at every step of its development.
“Every research trial that we run, we involve the patient community in the protocol,” Putrino says. This includes taking their advice on what trials should be prioritized, what symptoms to assess, how many clinic visits to require and what the testing environment should be like, to minimize the risk of exacerbating their symptoms, he says.
McCorkell says that the supplements she’s been taking have improved her general function by about 10%. Whereas that might not sound like much, she feels it is meaningful progress. Although the long COVID research has been difficult, she sees no other option but to stay involved. “We’re driven by desperation, out of improving our own quality of life.”