Yommie
SpeedLimited
- Oct 2, 2013
- 64,203
- 37,191
- Country of Origin

- Country of Residence

- Thread starter
- #556

COVID-19 shatters decades of global health progress, slashing life expectancy
Study in The Lancet reveals COVID-19 as the second leading cause of death in 2021, disrupting three decades of progress in global health and reducing life expectancy by 2.2 years from 2019 to 2021 despite previous gains.
COVID-19 shatters decades of global health progress, slashing life expectancy


A recent study published in The Lancet presented the global burden of 288 mortality causes and life expectancy decomposition.
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) has been analyzing causes of human death for over three decades, which has been used to guide policies, monitor/assess health interventions, and reduce risk factors. Assessing cause-specific mortality trends helps inform health policies, which must evolve to account for changes in the global health landscape.
Mortality patterns evolve continually as some areas succeed in reduction efforts while other causes linger in specific locations. Further, there have been improvements in several causes of death in the past three decades, some of which have substantially narrowed geographically and are concentrated in smaller areas.
 Study: Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Image Credit: tomertu / Shutterstock
Study: Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Image Credit: tomertu / ShutterstockAbout the study
In the present study, researchers presented mortality concentrations and life expectancy decomposition. GBD 2021 provided a comprehensive set of the fatal disease burden for 288 causes by sex and age in 204 countries and territories between 1990 and 2021, an update from previous estimates for 1990–2019. The team calculated years of life lost (YLLs) as the product of death count for each cause, age, sex, year, and location, as well as standard life expectancy at each age.Cause-specific mortality rates were computed using the causes of death ensemble model for most causes, and alternative strategies were applied to model causes with unusual epidemiology or insufficient data. Diseases and injuries were classified into four levels, with both non-fatal and fatal causes. Level 1 causes included three broad aggregate categories: 1) non-communicable diseases (NCDs), 2) communicable, maternal, neonatal, and nutritional (CMNN) diseases, and 3) injuries.
Level 2 disaggregated these categories into 22 clusters, which were further disaggregated into levels 3 and 4 causes. Life expectancy was decomposed by cause of death, year, and location to explore cause-specific effects on life expectancy between 1990 and 2021. Concentrated causes were estimated using the coefficient of variation and mortality concentration (the fraction of the population affected by 90% of deaths).
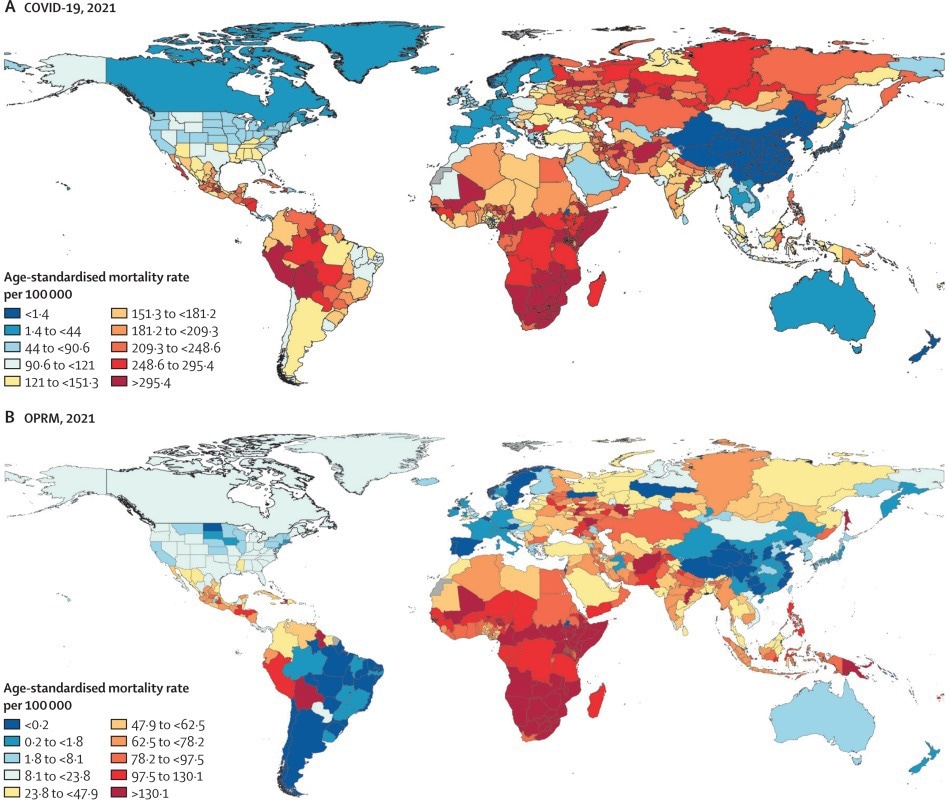
Global choropleth maps of COVID-19 (A) and OPRM (B) for 2021 that show sub-national detail where available. OPRM=other pandemic-related mortality.
Findings
During 1990–2019, the annual rate of change in all-cause global mortality ranged between -0.9% and 2.4%. The corresponding rate in age-standardized deaths ranged between -3.3 and 0.4%. Nevertheless, deaths increased by 10.8% worldwide in 2020 compared to 2019. This persisted in 2021, with a 7.5% increase relative to 2020. Likewise, the age-standardized mortality rate showed a similar pattern, increasing 8.1% in 2020 and 5.2% in 2021.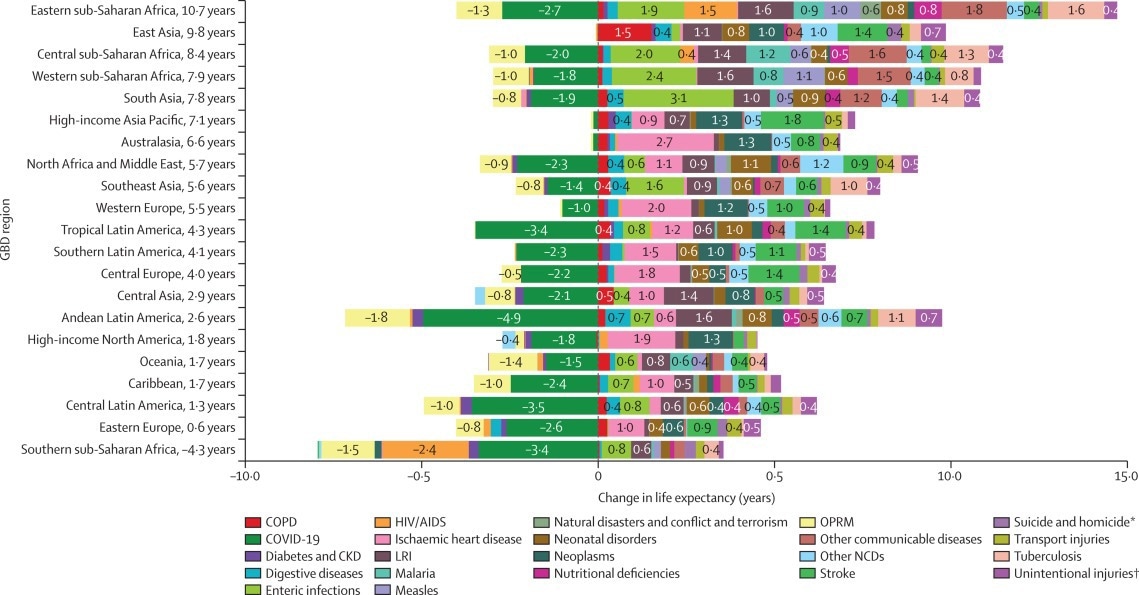
Related Stories
- How did COVID-19 impact cancer incidence trends in the US?
- Joint hypermobility linked to longer COVID-19 recovery time
- COVID-19 linked to higher dementia risk in older adults, study finds
In 2020-21, coronavirus disease 2019 (COVID-19) deaths and other pandemic-related mortality (OPRM) altered mortality patterns for the leading causes of age-standardized death. At level 3, the rankings of the four mortality causes (1. ischemic heart disease, 2. stroke, 3. chronic obstructive pulmonary disease, and 4. lower respiratory infections) with the highest age-standardized rates in 2019 were the same as in 1990.
However, in 2021, stroke became the third leading cause of age-standardized mortality, as COVID-19 eclipsed it as the second leading cause. Besides, OPRM was the fifth leading cause, whereas lower respiratory infections became the seventh leading cause. Although the impact of COVID-19 on age-standardized mortality was similar to that of common obstructive pulmonary disease in 2020, it increased by 60.2% in 2021.
Around 4.8 million and 7.89 million deaths occurred worldwide due to COVID-19 in 2020 and 2021, respectively. Age-standardized rates varied highly among GBD super-regions, with the highest in sub-Saharan Africa and the lowest in Southeast and East Asia and Oceania. OPRM and COVID-19 deaths also varied substantially by age, with older age groups being disproportionately affected.
In 1990, the three leading causes of YLLs globally were CMNN diseases. Further, neonatal disorders remained the leading cause in 2019, but NCDs, viz., ischemic heart disease and stroke, replaced the second and third leading causes, respectively. However, COVID-19 was the second leading cause of YLLs in 2021, with neonatal disorders and ischemic heart disease ranking first and third, respectively.
There have been long-standing positive trends in global life expectancy since the 1990s. Overall, life expectancy increased by 7.8 years between 1990 and 2019. However, during 2019-21, it decreased by 2.2 years due to COVID-19 and OPRM. Despite this decline, there was an overall increase of 6.2 years throughout the study period.
The decrease in mortality from enteric infections (paratyphoid, typhoid, and diarrheal diseases) affected the increase in global life expectancy. The reduction in deaths due to lower respiratory infection had the second most significant impact. All seven super-regions had an increase in life expectancy from 1990 to 2021.
Southeast and East Asia and Oceania had the highest gain (8.3 years), mainly due to lower mortality from chronic respiratory diseases. South Asia had the second largest gain (7.8 years) in life expectancy, mainly due to decreased mortality from enteric infections. Notably, Latin America and the Caribbean superregion had the largest decline in life expectancy (3.6 years) due to COVID-19.
The decline in mortality due to enteric disease substantially impacted global life expectancy. Mortality concentration emerged as 160 countries/territories made progress in CMNN disease mortality. Deaths were more concentrated in some regions or countries. For instance, 90% of deaths due to enteric infections in areas with 63% of the population of children under five years in 1990 reduced to areas with 51% of the population in 2021.
Further, the reduction in lower respiratory infections positively affected life expectancy in regions such as eastern and western sub-Saharan Africa and Andean Latin America. Moreover, reductions in stroke increased life expectancy by 0.8 years. However, stroke deaths were not concentrated. Overall, NCDs did not show a mortality concentration at large.
Conclusions
In sum, the present analysis offered insights into the global disease landscape before and during the two years of the COVID-19 pandemic. The findings showed that, after three decades of life expectancy improvements and reductions in age-standardized mortality rates, COVID-19 disrupted trends in the epidemiological transition, reversing long-standing progress.COVID-19 was the second leading age-standardized cause of death in 2021, profoundly impacting global life expectancy. It decreased life expectancy approximately as much as reductions in communicable diseases and NCDs have improved over decades. The study suggests that improved life expectancy outcomes could be achieved by leveraging past successes in mortality reduction.










 Why young men and women are drifting apartThe Economist
Why young men and women are drifting apartThe Economist Neuropathy is not from Low vitamin B. Meet the Real Enemy of Neuropathy (Stop Doing This)neuropathy.pro
Neuropathy is not from Low vitamin B. Meet the Real Enemy of Neuropathy (Stop Doing This)neuropathy.pro 'Never Paying for Prime'—Why 20,000 Users Prefer This Shopping SecretThis simple trick can save tons of money on Amazon, but most prime members are ignoring itonlineshoppingtools.com
'Never Paying for Prime'—Why 20,000 Users Prefer This Shopping SecretThis simple trick can save tons of money on Amazon, but most prime members are ignoring itonlineshoppingtools.com