Who needs Paxlovid now? New guidelines suggest only highest-risk groups should get COVID drug
Recommendations for provincial drug plans feature narrower definition of who should qualify
Lauren Pelley · CBC News · Posted: Apr 20, 2024 4:00 AM EDT | Last Updated: April 20
A Toronto intensive care unit in 2021, before the arrival of COVID-19 vaccines and treatments such as Paxlovid. There are new Canadian recommendations for who should actually get the antiviral at this point, guided by a growing body of research suggesting the drug’s life-saving benefits now apply to a narrower definition of high-risk individuals. (Evan Mitsui/CBC)
Social Sharing
- Facebook
- X
- Email
- Reddit
- LinkedIn
comments
This story is part of CBC Health's Second Opinion, a weekly analysis of health and medical science news emailed to subscribers on Saturday mornings. If you haven't subscribed yet, you can do that by clicking here.
If you consider yourself at a higher risk of serious illness from COVID-19 — because of your age, or maybe due to preexisting health issues — you might assume you'll be able to get treatment with Paxlovid when the time comes.
And you might assume the steep cost of the antiviral drug would be automatically covered by your provincial health plan.
But all that might change. There are new Canadian recommendations for who should actually get Paxlovid at this point, guided by a growing body of research suggesting the drug's life-saving benefits now apply to a narrower definition of high-risk individuals.
The expert committee for the Canadian Agency for Drugs and Technologies in Health (CADTH), the body providing advice for the country's publicly funded health care systems,
released draft recommendations earlier this year which offer fresh guidance for how drug plans should cover the treatment.
It stipulates Paxlovid should only be reimbursed for patients in two scenarios: If someone is severely immunosuppressed (such as organ transplant recipients) or moderately immunosuppressed (such as someone undergoing cancer treatment, individuals with advanced HIV infections, or anyone with moderate immunodeficiencies).
Simply being older or unvaccinated — both factors long thought to hike someone's risk of serious illness or death from COVID — didn't make the cut.
The recommendations were
provided to drug plans on April 11 as part of a negotiation process during which provinces decide whether or not to follow suit.
Multiple medical experts said if provincial decision makers do choose to align with the committee's suggestions, Canadians would only be eligible to get Paxlovid covered if they meet the narrow criteria for severe or moderate immunosuppression.
Those potential changes may come as a surprise to many Canadians who've long been eligible under broader provincial guidelines — including some that currently allow people
as young as 60 to
access the drug based on their age and other related risk factors.
But multiple experts told CBC News that who is truly high-risk now, four years into the pandemic, has changed. And narrowed eligibility is based on the latest research into how well the drug works for various groups, said University of British Columbia researcher Colin Dormuth, whose own findings helped inform the CADTH recommendations.
"The risk of something bad happening to you because of COVID-19 is now very low," Dormuth said.
WATCH | Concerns Paxlovid may not be reaching enough patients:
COVID drug Paxlovid may not be reaching enough patients
3 months ago
Duration2:17
Data from various provinces shows there is ample supply of Paxlovid — an antiviral drug meant to keep high-risk people with COVID out of hospitals — raising questions over whether enough patients who need it are getting it.
Who's most at risk has 'changed over time'
In the early years after SARS-CoV-2 first struck, the arrival of Pfizer's oral antiviral drug — a combination of the medications nirmatrelvir and ritonavir — was hailed as a game-changer.
But its rollout was marred by controversy. There were reports of symptom "rebound" after the five-day treatment,
which was later found to happen whether or not people took the drug. Some physicians also
questioned who actually benefited from Paxlovid as the pandemic evolved. And, perhaps not surprisingly given all that debate, there was often low uptake, which left
hundreds of thousands of treatments sitting unused across Canada.
Most recently, the federal government stopped its purchases of Paxlovid as of March 31, leaving future procurement up to the provinces. Most of Canada's remaining inventory also expired at the end of March, with a smaller portion expiring on May 31, said a spokesperson for the Public Health Agency of Canada.
Now multiple studies, including Dormuth's, are shedding light on where Pfizer's drug actually fits into the COVID treatment picture at this point in the pandemic.
Published in a
letter to members of the medical community from the University of British Columbia (UBC) Therapeutics Initiative, Dormuth's observational study looked at more than 6,000 B.C. residents. It showed Paxlovid was associated with reduced chance of severe illness in people at the highest risk, but found no evidence that it made a difference for anyone else.
"Even just within older people over 70, we didn't find an improvement in terms of reducing one's chance of being hospitalized or dying," Dormuth told CBC News.
"The bottom line is that for most people with COVID-19, Paxlovid will not make you feel better any faster, and will not lower your chance of [serious illness]."
The results, which have not been peer-reviewed, align with Pfizer's own findings. The drugmaker's latest trial data,
published in the New England Journal of Medicine earlier this month, looked at standard-risk groups — people who had risk factors and were vaccinated, along with unvaccinated individuals.
That trial found there weren't any major differences in COVID-related hospitalizations and deaths, nor was there any difference in how long people had symptoms, whether or not people had Paxlovid.
As of April 2024, the COVID-19 pandemic has caused more than seven million global deaths, making it the fifth-deadliest pandemic or epidemic in history. (Ivanoh Demers/Radio-Canada)
The Pfizer research also included participants of various ages. Age alone "is at best an arbitrary marker for risks … and needs to be contextualized among other risk factors such as vaccination status and comorbidities," wrote the Therapeutics Initiative team at UBC in their latest letter.
The draft CADTH guidelines for the province's drug plans also stressed that the risk factors involved in developing severe COVID once included a wide range of factors including older age, but "have changed over time" as population immunity increased.
Many experts now agree that widespread vaccination and prior infections helped the vast majority of people develop immunity to what was once a brand-new threat, reducing rates of serious illness. Vaccines are also thought to
dramatically ward off the possibility of developing long COVID.
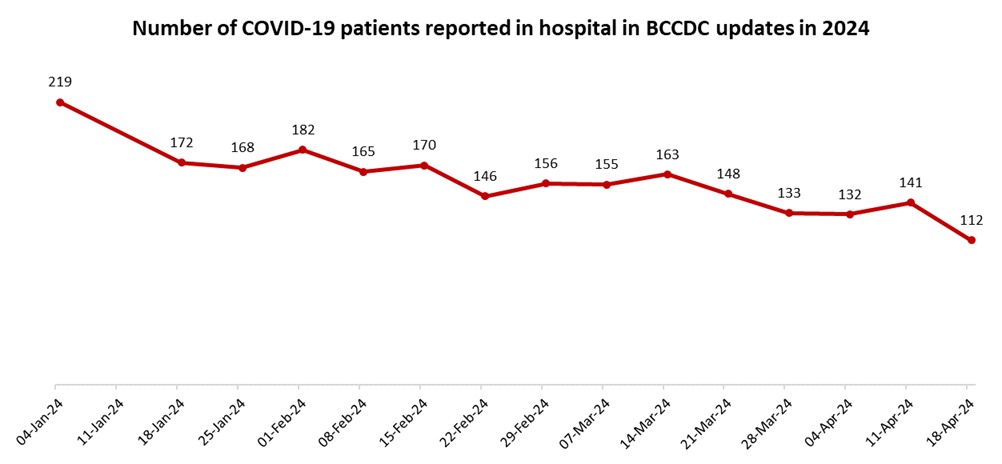
And in Canada, the number of patients dying of COVID
has plummeted, even among the oldest adults — though they still face highest rates of hospitalizations and ICU stays, which can erode someone's quality of life.
Drug still 'lifesaving' for high-risk individuals
It all paints a reassuring picture of this virus' trajectory.
Yet the grim reality is that deaths from COVID remain a routine occurrence, with more than 30 Canadians losing their lives
in the last week of March.
The question now is just how many of those deaths could be prevented — and whether the people who could benefit most from Paxlovid are the ones actually getting the drug.
U.S. infectious diseases physician Dr. Amesh Adalja, a senior scholar at the Johns Hopkins University Center for Health Security, also stressed Paxlovid was never designed to lessen people's symptoms in the general population, but rather to prevent severe disease.
And while it still works for that purpose, he warned misconceptions around the drug mean it ends up being under-prescribed in high-risk populations.
"'Keeping you alive' isn't resonating with people as much as 'decreasing your sore throat faster' or something like that," said Adalja.
"If people misunderstand what it does and it doesn't deliver on something that it was never designed to do, and people form a negative evaluation of the drug, that creates apprehension around prescribing it, and patients aren't asking their doctors for it."
WATCH | In 2022, thousands of Paxlovid doses went unused in Canada:
Thousands of doses of COVID-19 antiviral treatment remain unused
2 years ago
Duration2:02
Hundreds of thousands of doses of Paxlovid, a treatment for COVID-19, have gone unused in Canada because of difficulties in getting it to the right patients at the right time.
Adelja argued eligibility should remain more broad, allowing anyone with known risk factors — such as being 65 and up, pregnant, obese, or having other health issues or immunodeficiencies — to access the drug.
"Right now… Paxlovid is the best we have and it's really lifesaving for high-risk individuals," he said.
Anyone who considers themselves high risk should speak to their primary care provider about the drug if they do catch COVID, Dormuth said, adding he's concerned that people who truly need the drug might not be the ones accessing it in Canada.
In B.C. alone, roughly 300 people each week take Paxlovid, according to data cited by UBC's Therapeutics Initiative.
But with much less PCR testing and collection being done at this point in the pandemic, and no one collecting at-home rapid testing results, Dormuth said we've lost "critical data" to help understand who's getting sick and why.
'Resources aren't infinite' as drug costs $1,200+
The reality, he added, is "resources aren't infinite."
Pfizer's drug is pricey, costing $1,288.88 per five-day course, CADTH's documents show, prompting some experts to question if widespread purchasing and prescribing would actually save enough lives to justify those costs. (Should provinces no longer cover Paxlovid, it's also possible ineligible people may also have the option of paying out-of-pocket, or through private insurers, but again, it all depends on what each province decides.)
"As soon as we spend a dollar on one thing, we can't spend it on something else," Dormuth added.
With SARS-CoV-2 still circulating, multiple experts agreed that more front line treatments could come down the pike, making further studies into drug efficacy essential.
"We definitely continue to need more research on what treatments actually work for COVID in the acute phase, and we still don't have that evidence," said Unity Health public health specialist Dr. Andrew Pinto, the director of the University of Toronto's
Upstream Lab.
Pinto is part of a Canadian team doing ongoing research into Paxlovid and other existing and future treatments through the cross-country
CanTreatCOVID trials, which have so far enrolled roughly 450 participants.
The goal, he said, is eventually pooling results with the larger
PANORAMIC trials happening in the U.K.
"COVID is still with us, and will likely continue to be with us," he said. "It's still quite a deadly disease compared to other respiratory infections."



































 Pix for representational purpose only/REUTERSPix
Pix for representational purpose only/REUTERSPix